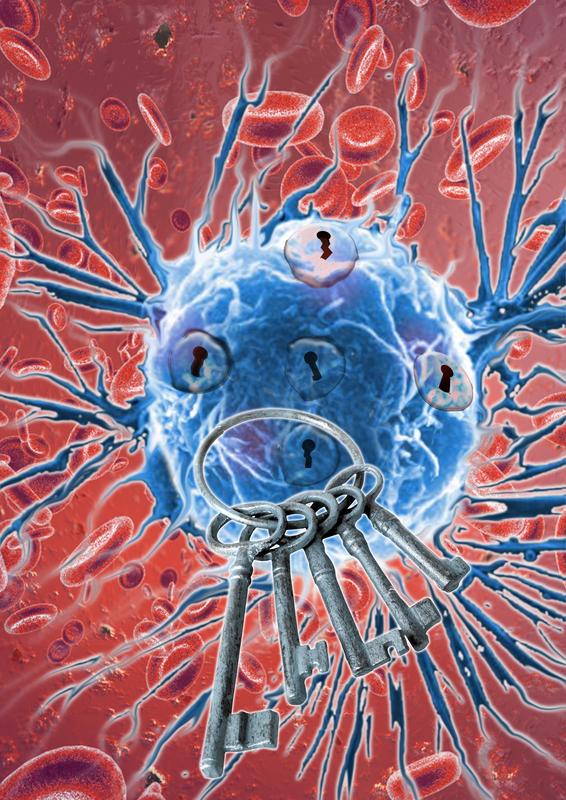
Targeted agents are thought to be keys to better cancer therapy. Cancer cells can adapt to targeted therapies, so the best key combination can change over time.
IMP
Over the past years, scientists have drawn an almost complete map of mutations in cancer. However, translating complex genetic knowledge into effective cancer therapies turns out to be a major challenge for modern medicine.
Searching for new ways to attack cancer cells, the laboratory of Johannes Zuber at the IMP in Vienna uses so-called functional genetic screens to probe vulnerabilities of cancer cells in a systematic and unbiased way. The major goal is to find genes that cancer cells particularly depend on, and then exploit these “Achilles’ heels” for the development of targeted therapies.
In a first study applying this technology, Zuber and his former colleagues at Cold Spring Harbor Laboratory (New York) in 2011 found that the gene BRD4 is such an “Achilles’ heel” in acute myeloid leukemia (AML), an aggressive form of blood cancer. This discovery sparked a lot of excitement about BRD4 as a new target for leukemia therapy, and only four years later several BRD4 inhibitors have entered clinical trials, some of which have already reported promising results.
Resistance to new cancer therapies is often poorly understood
Despite this rapid advance, doctors and researchers still do not understand why some cancers are so sensitive to BRD4 inhibitors while others remain resistant. “After discovering a new Achilles’ heel, we often have no clue why cancer cells depend on a certain gene, although this knowledge would be crucial for developing targeted therapies and selecting the right patients”, explains Zuber. In the case of BRD4, finding an answer to this question turned out to be particularly challenging.
To tackle this problem, Zuber and his group at the IMP teamed up with previous co-workers in the U.S. and scientists at Boehringer Ingelheim in Vienna led by Norbert Kraut to characterize sensitive and resistant cancer cells. Results from this work have been published in Nature and reveal a fascinating new mechanism how leukemia cells evade their dependency on BRD4.
As a known regulator of transcription, BRD4 controls the activity of hundreds of genes, which are simultaneously turned off after inhibitor treatment. In leukemia, one particularly important gene controlled by BRD4 is the MYC oncogene, which leukemia cells need for their indefinite growth. Treatment with BRD4 inhibitors shuts off this important cancer gene, and leukemia cells either die or develop into normal blood cells.
To better understand why only certain leukemia subtypes are sensitive to BRD4 inhibition, Zuber and his colleagues first performed a genetic screen and found that loss of the so called PRC2 complex, which is known to inactivate genes during normal development, can render leukemia cells resistant to BRD4 inhibitors. By further characterizing these cells they found out that MYC and other BRD4-regulated genes were back on again, so leukemia cells had found a way to activate these genes in the absence of BRD4.
Cancer cells “learn” to evade the effects of BRD4 inhibitors
When the researchers then compared cells that had acquired resistance during drug treatment to leukemia cells that were resistant in the first place, they found that in both cases leukemia cells use very similar pathways to turn critical genes such as MYC back on and thereby escape the deadly effects of BRD4 inhibition. “It looked as if sensitive leukemia cells just learned what resistant cells already knew”, explains postdoctoral scientist Philipp Rathert, who spearheaded the study together with Mareike Roth, a graduate student in the Zuber laboratory. One particularly important pathway turned out to be WNT signalling, which is known to activate MYC in colon cancer and other cancer subtypes.
To look at the regulation of MYC in even more detail, Zuber was able to take advantage of close interactions with Alexander Stark at the IMP, whose laboratory has recently developed a method called “STARR-seq”. This technology has revolutionised the study of so-called enhancers, which are DNA regions involved in gene regulation. Using this new method, the team found that resistant leukemia cells activate MYC through a very small enhancer region that is bound by WNT components and gains activity following BRD4 inhibition.
A new biomarker to predict success of leukemia therapy
To explore whether this detailed knowledge could be used to predict which patients respond to BRD4 inhibitors, the team harnessed a long-standing collaboration with the group of Peter Valent at the Medical University of Vienna. When measuring WNT signalling markers, the team found that patient cells with low WNT activity were sensitive to BRD4 inhibitors, while high WNT activity was associated with resistance. This means the researchers may hold in hands a first “biomarker” for predicting the success of BRD4 inhibitor therapy.
Collectively, the study reveals that leukemia cells can become resistant to BRD4 inhibitors by rewiring the regulation of critical BRD4 target genes. This “transcriptional plasticity” highlights an emerging mode of drug resistance that is distinct from established resistance mechanisms such as mutations in binding pockets or drug elimination through efflux pumps. While this showcases once more that cancer cells can adapt to targeted therapies, Zuber and his colleagues at the IMP and Boehringer Ingelheim believe that a better understanding of these adaptation mechanisms will lead to combination therapies that will ultimately outsmart cancer cells: “We now have learned that cancer cells can adapt to targeted therapies, but their repertoire of escape routes is quite limited”, comments Zuber on the implications of their study. “A better understanding of the common escape routes will allow us to predict the next effective targeted therapy, so that we are always one step ahead of the cancer cell.”
The Research Institute of Molecular Pathology (IMP) in Vienna is a basic biomedical research institute that is located at the Vienna Biocenter and largely sponsored by Boehringer Ingelheim. With over 200 scientists from 35 nations, the IMP is committed to scientific discovery of fundamental molecular and cellular mechanisms underlying complex biological phenomena. Norbert Kraut, global head of oncology research at Boehringer Ingelheim, believes that the joint work on BRD4 is a particularly remarkable example of an academia-industry collaboration resulting in a key biomedical discovery. “The Boehringer Ingelheim-IMP collaboration has now been successfully developing over the past more than 20 years. Collaborative spirit, outstanding networking skills and open innovation from all partners were key in this joint effort to comprehensively understand how cancer cells can evade the promising class of clinical-stage BRD4/BET family inhibitors. Examples like this illustrate that the Boehringer Ingelheim-IMP collaboration continues to yield new therapeutic concepts that may impact future clinical trials towards improved cancer precision therapies.”
Johannes Zuber was born in Dresden in 1974. In 2001 he finished his medical studies at the Humboldt University in Berlin, followed by a doctoral degree in molecular cancer research in 2003. During his residency as a medical doctor at Charité University Hospital, leukemia became the focus of his clinical and scientific work. In 2005, he moved to the U.S. to join Scott Lowe’s laboratory in Cold Spring Harbor (New York), and in 2011, he became a group leader at the IMP in Vienna. By combining genetically engineered cancer models and advanced genetic screening approaches, Johannes Zuber and his team explore cancer-specific vulnerabilities (so-called “non-oncogene addictions”) in a systematic and unbiased way.
Publication:
The paper “Transcriptional plasticity promotes primary and acquired resistance to BET inhibition” by Rathert & Roth et al. was published online by Nature on September 14, 2015 (DOI 10.1038/nature14898).
Illustration:
lllustrations to accompany this press release can be downloaded from the IMP-Website: www.imp.ac.at/pressefoto-targetedtherapy
Contact:
Dr. Heidemarie Hurtl
IMP Communications
hurtl@imp.ac.at
+43 (0)1 79730 3625