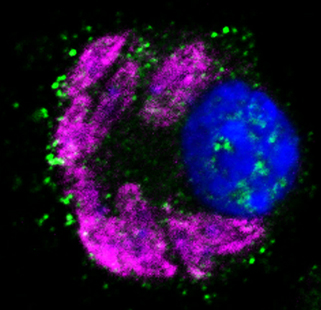
Macrophages (blue nucleus) that are infected with Leishmania major (purple) and have been stimulated with the messenger substance interleukin 4 produce arginase 1 (green).
Katrin Paduch/FAU Institute of Microbiology
In order to defend the body against intracellular pathogens, such as the single-cell parasites Leishmania major, nitric oxide (NO) must be produced. This is formed in macrophages and other phagocytes through type 2 NO synthase (NOS2).
However, the function of NOS2 is inhibited by a competing enzyme called arginase 1. The researchers, led by PD Dr. Ulrike Schleicher and Prof. Dr. Christian Bogdan at FAU’s Institute of Microbiology – Clinical Microbiology, Immunology and Hygiene, demonstrated through cell culture experiments and an infection model that tumour necrosis factor inhibits arginase 1 synthesis, which depends on the messenger substance interleukin 4. This causes nitric oxide production to increase and suppresses the pathogens.
‘As long as they can be confirmed in ongoing experiments with human cells, these findings provide a plausible explanation of the increased susceptibility to infection that occurs during anti-TNF treatments,’ explains Professor Bogdan, ‘In the future, concurrent use of arginase 1 inhibitors could minimise the risk of infection associated with TNF inhibition.’
The results of the study, which was partially carried out in the framework of FAU’s Interdisciplinary Centre for Clinical Research and DFG Collaborative Research Centre 1181, have recently been published in the international journal Cell Reports (DOI: 10.1016/j.celrep.2016.04.001)
Further information:
Prof. Dr. Christian Bogdan
Phone: +49 9131 8522551
christian.bogdan@uk-erlangen.de