
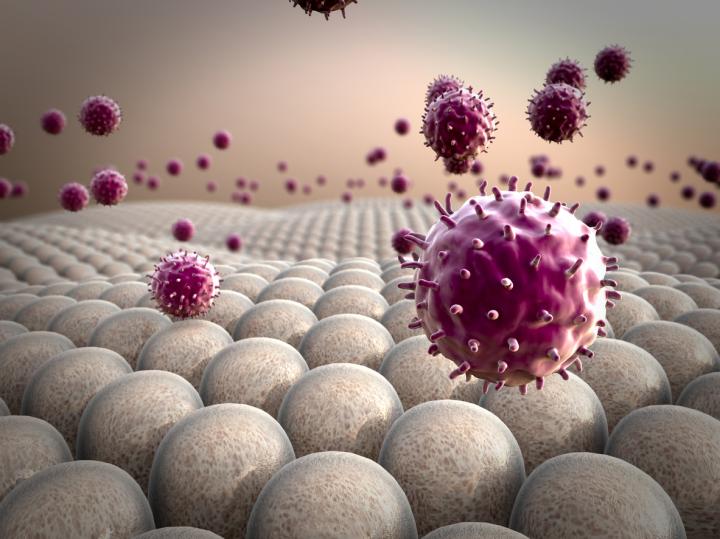
A rendering of a macrophage
Credit: Penn Medicine
Chimeric antigen receptor (CAR) T cell therapy has been a game-changer for blood cancers but has faced challenges in targeting solid tumors. Now researchers from the Perelman School of Medicine at the University of Pennsylvania may have an alternative to T cell therapy that can overcome those challenges.
Their research shows genetically engineering macrophages – an immune cell that eats invaders in the body – could be the key to unlocking cellular therapies that effectively target solid tumors.
The team was able to show these CAR macrophages can kill tumors both in human samples in the lab and in mouse models. They published their proof-of-concept paper in Nature Biotechnology today.
The approach in this study is closely related to CAR T cell therapy, in which patient immune cells are engineered to fight cancer, but it has some key differences.
Most importantly, it centers around macrophages, which eat invading cells rather than targeting them for destruction the way T cells do; while T cells are more like a game of Space Invaders, macrophages are like Pac-Man.
Macrophages also have another key difference from T cells in that they are the body's first responders to viral infections. This has historically presented challenges in trying to engineer them to attack cancer, since macrophages are resistant to infection by the standard viral vectors used in gene and cell therapy.
“We have known how to engineer T cells to do this for years, but the fact that macrophages are innately resistant to the viral vectors that we use in our CAR T cells presented a unique challenge, which we show here we were able to overcome,” said the study's senior author Saar Gill, MD, PhD, an assistant professor of Hematology-Oncology and a member of Penn's Abramson Cancer Center.
In fact, this anti-viral property carried another unexpected benefit. Macrophages are generally among the first cells to be drawn in by cancer, and they are exploited to help tumors instead of eating them.
However, the research team showed that when the viral vector is inserted, not only do these engineered macrophages express the CAR, they also transform into highly inflammatory cells. This transformation allows macrophages to resist being co-opted by tumors.
Researchers say CAR macrophages may also be able to stimulate the rest of the immune system as they attack, potentially opening the door to a greater immune response.
“Finding ways to draw the rest of the body's powerful immune system into the fight would mean an even greater impact than what a cellular therapy can do on its own, so our future research will include efforts to better understand this possibility and how we might be able to exploit it to kill cancer,” said the study's first author Michael Klichinsky, PhD, who was a graduate student at Penn while he completed the work. This paper represents the culmination of his graduate career in Gill's lab. Klichinsky and Gill went on to co-found a company, Carisma Therapeutics, based on the CAR Macrophage approach.
###
Additional Penn authors include, Marco Ruella, Olga Shestova, Xueqing Maggie Lu, Nicholas Petty, Katherine Cummins, Feng Shen, Xinhe Shan, Kimberly Veliz, Kristin Blouch, Saad S. Kenderian, Miriam Y. Kim, Roddy O'Connor, Stephen Wallace, Miroslaw S. Kozlowski, Dylan M. Marchione, Maksim Shestov, Benjamin A. Garcia, and Carl June.
Editor's Note: Klichinsky and Gill are scientific co-founders of Carisma Therapeutics and hold equity in the company. Klichinsky is currently Vice President of Discovery Research at Carisma Therapeutics. Klichinsky, Gill, and June are members of the company's scientific advisory board and are inventors on intellectual property related to this work and may receive additional financial benefits in the future. Penn is also an investor in the company and holds equity interests.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $7.8 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $425 million awarded in the 2018 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center–which are recognized as one of the nation's top “Honor Roll” hospitals by U.S. News & World Report–Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; and Pennsylvania Hospital, the nation's first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Home Care and Hospice Services, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is powered by a talented and dedicated workforce of more than 40,000 people. The organization also has alliances with top community health systems across both Southeastern Pennsylvania and Southern New Jersey, creating more options for patients no matter where they live.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2018, Penn Medicine provided more than $525 million to benefit our community.












