
Preserving Retinal Photoreceptors After Injury: New Research Insights
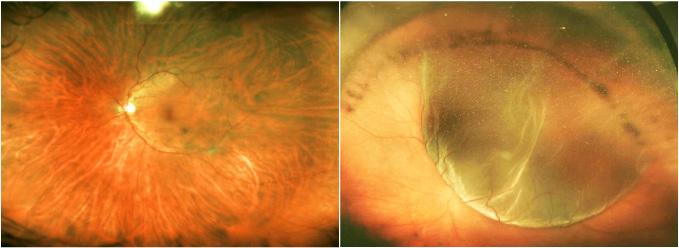
Left, an image of a human retina from a healthy individual. Right, a retinal image from a patient with a retinal detachment. Note the balloon like structure of the retinal detachment.
(Image courtesy of Dr. Leo A. Kim, Massachusetts Eye and Ear Infirmary)
Vision researchers at Massachusetts Eye and Ear/Harvard Medical School (HMS) Department of Ophthalmology have taken a first step in solving a vexing problem: how to preserve photoreceptor cells and avoid irreversible vision loss in patients following retinal detachment.
Degeneration of photoreceptors, the major light-sensing cells in the eye, is a primary cause of vision loss worldwide. Identifying the underlying causes surrounding photoreceptor cell death is paramount in order to develop new treatment strategies to prevent their loss. Retinal detachment and subsequent degeneration of the retina can lead to progressive visual decline due to photoreceptor cell death. Since photoreceptors are non-dividing cells, their loss results in irreversible visual impairment even after successful retinal reattachment surgery.
New research led by Kip M. Connor, Ph.D., a researcher and Assistant Professor of Ophthalmology at Mass. Eye and Ear/HMS Ophthalmology and colleagues analyzed innate immune system regulators in the eyes of human patients with retinal detachment and correlated their findings in an experimental model. They discovered that there was a significant increase in the immune system's 'alternative complement pathway' following retinal detachment and that this pathway facilitated early photoreceptor cell death after injury.
Injured photoreceptors lose important proteins that normally protect them from complement mediated cell death, allowing for selective targeting by the alternative complement pathway. Additionally, by blocking the alternative complement pathway, through both genetic and pharmacologic means, photoreceptors were protected from cell death.
“When photoreceptors in a detached retina were removed from their primary source of oxygen and nutrients, we found an increase in complement factor B?a key mediator of the alternative complement pathway that leads to photoreceptor cell death,” says Dr. Connor. “For the first time these results provide evidence that the alternative complement pathway exacerbates photoreceptor cell death and that inhibition of the pathway is protective,” said Kaylee Smith, a member of the Connor Lab and contributing author on the manuscript. Their findings were published today in the journal, Science Translational Medicine.
Retinal detachment can occur as a result of either blunt trauma or as a side effect of a variety of eye diseases, including diabetic retinopathy, ocular tumors, and age-related macular degeneration. The current standard of care is surgical reattachment, with patients in the United States and Europe typically treated within one week of the injury. Today's state-of-the-art surgical techniques are highly effective at physically reattaching the retina and?if surgery is timely?a positive, visual outcome often results. Even so, patients often complain of permanent vision loss accompanied by changes in color vision. “Studies in both humans and animal models have shown that photoreceptor cell death is induced as early as 12 hours after detachment, indicating that early intervention could potentially preserve photoreceptors and improve the visual function of patients who undergo reattachment surgery. Our research provides a new role for complement in retinal detachment, and suggests that inhibition of the alternative complement pathway may be good therapeutic target to prevent the initial photoreceptor cell loss,” notes Dr. Connor.
“What makes this research so exciting is the potential impact it can have on our patients,” he adds. “Working closely with our colleagues in the clinic, we identified a challenging issue, went back to our laboratories to uncover a cause, and now have knowledge that may help us to develop therapies that will help to preserve our patients' vision.”
###
Funding notes:
Research reported in this [publication/press release] was supported by National Eye Institute of the National Institutes of Health under award numbers: R01EY022084/S1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Generous awards from Research to Prevent Blindness (RPB): RPB Special Research Scholar Award to Kip M. Connor, RPB Physician-Scientist Award to Demetrios Vavvas and an Unrestricted Grant to the Department of Ophthalmology, Harvard Medical School, Joan W. Miller, Chair.
About Massachusetts Eye and Ear
Mass. Eye and Ear clinicians and scientists are driven by a mission to find cures for blindness, deafness and diseases of the head and neck. After uniting with Schepens Eye Research Institute Mass. Eye and Ear in Boston became the world's largest vision and hearing research center, offering hope and healing to patients everywhere through discovery and innovation. Mass. Eye and Ear is a Harvard Medical School teaching hospital and trains future medical leaders in ophthalmology and otolaryngology, through residency as well as clinical and research fellowships. Internationally acclaimed since its founding in 1824, Mass. Eye and Ear employs full-time, board-certified physicians who offer high-quality and affordable specialty care that ranges from the routine to the very complex. U.S. News & World Report's “Best Hospitals Survey” has consistently ranked the Mass. Eye and Ear Departments of Otolaryngology and Ophthalmology as top five in the nation.
About Harvard Medical School Department of Ophthalmology
The Harvard Medical School (HMS) Department of Ophthalmology is one of the leading and largest academic departments of ophthalmology in the nation. More than 350 full-time faculty and trainees work at nine HMS affiliate institutions, including Massachusetts Eye and Ear/Schepens Eye Research Institute, Massachusetts General Hospital, Brigham and Women's Hospital, Boston Children's Hospital, Beth Israel Deaconess Medical Center, Joslin Diabetes Center/Beetham Eye Institute, Veterans Affairs Boston Healthcare System, VA Maine Healthcare System, and Cambridge Health Alliance. Formally established in 1871, the department has been built upon a strong and rich foundation in medical education, research, and clinical care. Through the years, faculty and alumni have profoundly influenced ophthalmic science, medicine, and literature–helping to transform the field of ophthalmology from a branch of surgery into an independent medical specialty at the forefront of science.
CONTACT: Joseph O'Shea
joseph_oshea@meei.harvard.edu
617-573-3341












