3-D printing techniques help surgeons carve new ears
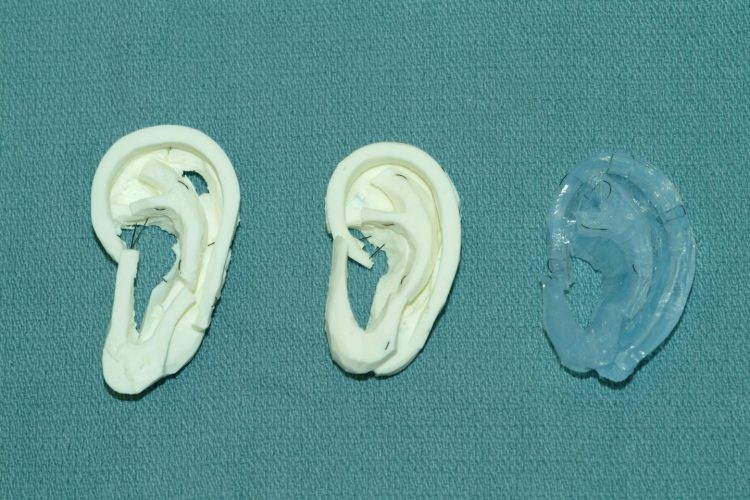
In the study, experienced surgeons preferred carving the UW's models (in white) over a more expensive material made of dental impression material (in blue). Credit: University of Washington
To treat children with a missing or under-developed ear, experienced surgeons harvest pieces of rib cartilage from the child and carve them into the framework of a new ear. They take only as much of that precious cartilage as they need.
That leaves medical residents without an authentic material to practice on, as vegetables are a pale substitute. Some use pig or adult cadaver ribs, but children's ribs are a different size and consistency.
Now, a collaboration between a University of Washington otolaryngology resident and bioengineering student has used 3-D printing to create a low-cost pediatric rib cartilage model that more closely resembles the feel of real cartilage and allows for realistic surgical practice. The innovation could open the door for aspiring surgeons to become proficient in the sought-after but challenging procedure.
Their results are described in an abstract presented this week at the American Academy of Otolaryngology — Head and Neck Surgery conference in Dallas.
“It's a huge advantage over what we're using today,” said lead author Angelique Berens, a UW School of Medicine otolaryngology — head and neck surgery resident. “You literally take a bar of Lever 2000 while the attending is operating and you carve ear cartilage. It does teach you how to get the shape right, but the properties are not super accurate — you can't bend it, and sewing it is not very lifelike.”
As part of the study, three experienced surgeons practiced carving, bending and suturing the UW team's silicone models, which were produced from a 3-D printed mold modeled from a CT scan of an 8-year-old patient. They compared their firmness, feel and suturing quality to real rib cartilage, as well as a more expensive material made out of dental impression material.
All three surgeons preferred the UW models, and all recommended introducing them as a training tool for surgeons and surgeons-in-training.
Kathleen Sie, a UW Medicine professor of otolaryngology — head and neck surgery and director of the Childhood Communication Center at Seattle Children's, said the lack of adequate training models makes it difficult for people to become comfortable performing the delicate and technical procedure, which is called auricular reconstruction.
There's typically a six- to 12-month waiting list for children to have the procedure done at Seattle Children's, she said.
“It's a surgery that more people could do, but this is often the single biggest roadblock,” Sie said. “They're hesitant to start because they've never carved an ear before. As many potatoes and apples as I've carved, it's still not the same.”
Another advantage is that because the UW models are printed from a CT scan, they mimic an individual's unique anatomy. That offers the opportunity for even an experienced surgeon to practice a particular or tricky surgery ahead of time on a patient-specific rib model.
Co-author Sharon Newman, who graduated from the UW with a bioengineering degree in June, teamed up with Berens while they both worked in the UW BioRobotics Lab under electrical engineering professor Blake Hannaford.
Newman figured out how to upload and process a CT scan through a series of free, open-source modeling and imaging programs, and ultimately use a 3-D printer to print a negative mold of a patient's ribs.
Newman had previously tested different combinations of silicone, corn starch, mineral oil and glycerin to replicate human tissue that the lab's surgical robot could manipulate. She poured them into the molds and let them cure to see which mixture most closely resembled rib cartilage.
“I would go to the craft store and Home Depot and say I want to make models — what aisle should I go to?” said Newman. “It turns out a lot of these ideas were based off of materials people use for arts and crafts like rings or other jewelry.”
The team's next steps are to get the models into the hands of surgeons and surgeons-in-training, and hopefully to demonstrate that more lifelike practice models can elevate their skills and abilities.
“With one 3-D printed mold, you can make a billion of these models for next to nothing,” said Berens. “What this research shows is that we can move forward with one of these models and start using it.”
###
Co-authors include Craig Murakami, UW clinical associate professor and Virginia Mason Medical Center otolaryngologist — head and neck surgeon and facial plastic surgeon, and David A. Zopf, assistant professor of otolaryngology — head and neck surgery at the University of Michigan.
For more information, contact Berens at berens@uw.edu or 616-291-8206.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Innovative vortex beam technology
…unleashes ultra-secure, high-capacity data transmission. Scientists have developed a breakthrough optical technology that could dramatically enhance the capacity and security of data transmission (Fig. 1). By utilizing a new type…

Tiny dancers: Scientists synchronise bacterial motion
Researchers at TU Delft have discovered that E. coli bacteria can synchronise their movements, creating order in seemingly random biological systems. By trapping individual bacteria in micro-engineered circular cavities and…

Primary investigation on ram-rotor detonation engine
Detonation is a supersonic combustion wave, characterized by a shock wave driven by the energy release from closely coupled chemical reactions. It is a typical form of pressure gain combustion,…



