Prediabetes: Fatty Liver, Visceral Obesity, impaired Production and Action of Insulin modulate Risk
Source: Stefan et al. Phenotypes of prediabetes and stratification of cardiometabolic risk. Lancet Diabetes & Endocrinology 2016. © The Lancet Diabetes & Endocrinology
In many countries the prevalence of diabetes and prediabetes has reached epidemic numbers. In the USA and in China more than half of the adult population already has elevated blood glucose levels. Worrisome is that already in the state of prediabetes hyperglycemia is associated with increased risk of type 2 diabetes, cardiovascular disease, dementia and cancer.
However, the disease risk considerably varies even in the state of prediabetes. This lead scientists at the Department of Internal Medicine IV of the University Hospital of Tübingen and of the Institute of Diabetes Research and Metabolic Diseases (IDM) of the Helmholtz Center Munich, partners of the German Center for Diabetes Research (DZD), to study what parameters may explain this variability in disease risk in prediabetes.
Type 2 diabetes is a very heterogeneous disease
Among scientists it is well established that several pathophysiological mechanisms are involved in the development of type 2 diabetes. However, in a clinical setting it is very difficult to disentangle these mechanisms which may be very useful to implement a personalized prevention and treatment of diabetes.
The relevance to account for the major pathophysiological mechanisms of diabetes can be observed that in diabetes diagnosed by elevated fasting or 2 hr glucose levels during a standard oral glucose tolerance test (OGTT) the prevalence and the sequence of appearance of impaired insulin production and impaired insulin secretion differ. This variability in the prevalence of these risk phenotypes can already be observed in the prediabetic states isolated impaired fasting glucose (IFG), isolated impaired glucose tolerance (IGT) or IFG+IGT combined.
At-Risk Phenotypes predict prediabetes and cardiovascular risk
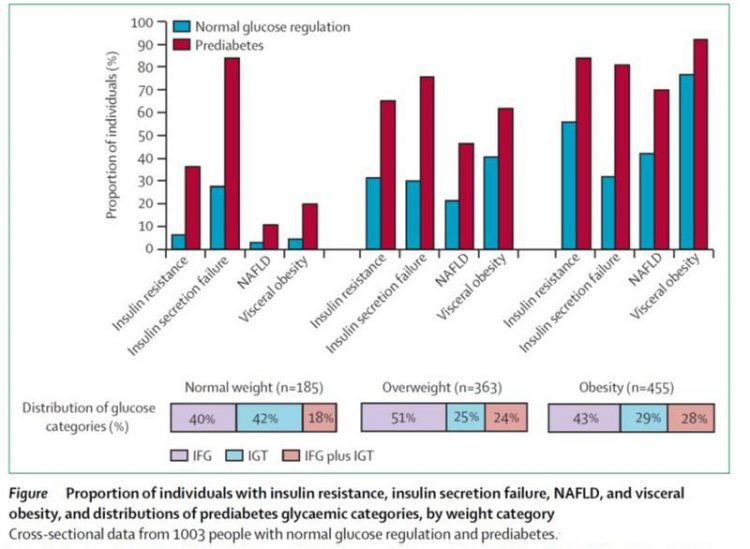
In an analysis of data from 1003 subjects of the Tübingen Diabetes Family Study of whom 405 had prediabetes, the 4 at risk phenotypes insulin secretion failure, insulin resistance, fatty liver, and magnetic-resonance imaging (MRI)-determined visceral obesity, but not BMI category (normal weight, overweight, and obese) or visceral obesity based on waist circumference, were independent determinants of prediabetes.
Except for visceral obesity, the other 3 at risk-phenotypes also predicted the regression from prediabetes to normal glucose regulation (NGR) during a lifestyle intervention. Among the individuals with prediabetes, fatty liver was the strongest determinant of increased carotid intima–media thickness, an early marker of atherosclerosis, followed by MRI-determined visceral obesity.
Phenotypes of prediabetes
Based on the emerging evidence for the existence of the very interesting extreme metabolic phenotypes metabolically healthy obesity and metabolically unhealthy normal weight the scientist then studied the prevalence of the 4 at-risk phenotypes among the different BMI categories (normal weight, overweight, and obese) in subjects with NGR and prediabetes.
They could show that there are distinct signatures of these phenotypes among these BMI categories (figure). For example, while insulin secretion failure is by far the most prevalent at-risk phenotype in normal weight subjects with prediabetes, fatty liver and visceral obesity become more prevalent in overweight and obese subjects.
Conclusion: Phenotypes of prediabetes should be consideration in prevention and treatment of cardiometabolic diseases
Norbert Stefan, the first author of the article, proposes that ‘after initial classification of the glucose categories NGR and prediabetes, fatty liver, visceral obesity and impaired production and action of insulin should be included in assessment of cardiometabolic risk. If proven to be effective, this strategy could be included in medical guidelines about the prevention and treatment of diabetes and associated diseases’. Hans Häring, the last author of the study adds ‘the application of precise phenotyping strategies in clinical trials will also help to improve understanding of the pathophysiology of cardiometabolic diseases.’
Source
Norbert Stefan, Andreas Fritsche, Fritz Schick, Hans-Ulrich Häring. Phenotypes of prediabetes and stratification of cardiometabolic risk. Lancet Diabetes & Endocrinology 2016 [epub ahead of print] DOI: http://dx.doi.org/10.1016/S2213-8587(16)00082-6
The German Center for Diabetes Research (DZD) is a national association that brings together experts in the field of diabetes research and combines basic research, translational research, epidemiology and clinical applications. The aim is to develop novel strategies for personalized prevention and treatment of diabetes. Members are Helmholtz Zentrum München – German Research Center for Environmental Health, the German Diabetes Center in Düsseldorf, the German Institute of Human Nutrition in Potsdam-Rehbrücke, the Paul Langerhans Institute Dresden of the Helmholtz Zentrum München at the University Medical Center Carl Gustav Carus of the TU Dresden and the Institute for Diabetes Research and Metabolic Diseases of the Helmholtz Zentrum München at the Eberhard-Karls-University of Tuebingen together with associated partners at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich. More information: www.dzd-ev.de/en
The Helmholtz Zentrum München, the German Research Center for Environmental Health, pursues the goal of developing personalized medical approaches to the prevention and therapy of major common diseases such as diabetes and lung disease. To achieve this, it investigates the interaction of genetics, environmental factors and lifestyle. The Helmholtz Zentrum München has about 2,300 staff members and is headquartered in Neuherberg in the north of Munich. It is a member of the Helmholtz Association, a community of 18 scientific-technical and medical-biological research centers with a total of about 37,000 staff members. The Helmholtz Zentrum München is a partner in the German Center for Diabetes Research.
Media contact
Dr. Astrid Glaser
German Center for Diabetes Research (DZD)
Ingolstädter Landstr. 1
85764 Neuherberg
Germany
Phone: 089-3187-1619
Email: contact@dzd-ev.de
www.dzd-ev.de
Contact for inquiries about the current publication
Prof. Dr. med. Norbert Stefan
Tübingen University Hospital
Department of Internal Medicine IV
Otfried-Müller-Straße 10, 72076 Tübingen
Germany
Phone: +49 (0)7071 29-80390
Email: norbert.stefan@med.uni-tuebingen.de
https://www.dzd-ev.de/en/index.html
https://twitter.com/DiabResearch
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

A ‘language’ for ML models to predict nanopore properties
A large number of 2D materials like graphene can have nanopores – small holes formed by missing atoms through which foreign substances can pass. The properties of these nanopores dictate many…

Clinically validated, wearable ultrasound patch
… for continuous blood pressure monitoring. A team of researchers at the University of California San Diego has developed a new and improved wearable ultrasound patch for continuous and noninvasive…

A new puzzle piece for string theory research
Dr. Ksenia Fedosova from the Cluster of Excellence Mathematics Münster, along with an international research team, has proven a conjecture in string theory that physicists had proposed regarding certain equations….



