Novel MRI-guided ultrasound treatment destroys prostate cancer
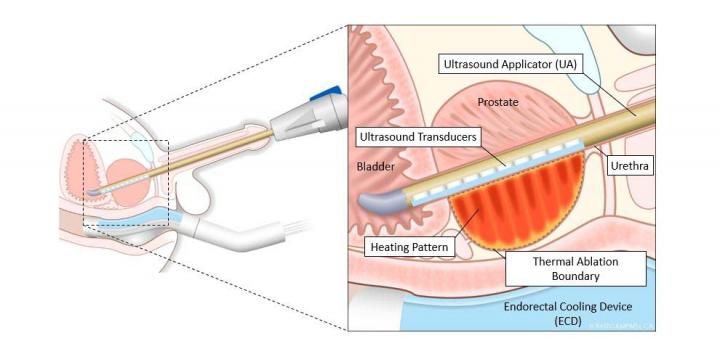
This diagram shows controlled and precise ablation using TULSA-PRO®. Credit: Study author and RSNA
Prostate cancer is the second-leading cause of cancer death in men after lung cancer. Treating disease in the small gland that surrounds the urethra just outside the bladder is challenging.
Surgery and radiation are not always effective and can result in incontinence, impotence and bowel dysfunction. Other currently available techniques lack sophisticated imaging guidance and temperature monitoring.
In recent years, a minimally invasive method called MRI-guided transurethral ultrasound ablation (TULSA) has emerged as a promising treatment option. TULSA works by delivering precise doses of sound waves to diseased prostate tissue while sparing the healthy nerve tissue surrounding the prostate.
TULSA relies on a rod-shaped device that is inserted into the urethra. The novel device has 10 ultrasound-generating elements that can cover the entire prostate gland. One or more of the elements are used to send out sound waves that heat and destroy the target prostate tissue.
The elements are controlled automatically by a software algorithm that can adjust the shape, direction and strength of the therapeutic ultrasound beam. The entire procedure takes place in an MRI scanner so that doctors can closely monitor treatment and assess the degree and location of heating.
“Unlike with other ultrasound systems on the market, you can monitor the ultrasound ablation process in real time and get immediate MRI feedback of the thermal dose and efficacy,” said study co-author Steven S. Raman, M.D., professor of radiology and urology, and director of Prostate MR Imaging and Interventions and Prostate MR Imaging Research at the University of California at Los Angeles (UCLA). “It's an outpatient procedure with minimal recovery time.”
In the new multicenter study, researchers reported on the 12-month outcomes from the TULSA-PRO® ablation clinical trial (TACT). The trial enrolled 115 men, median age 65, with localized low or intermediate risk, gland-confined prostate cancer. Clinicians delivered TULSA treatment to the entire gland. Treatment time averaged 51 minutes.
Prostate volume in the study group decreased on average from 39 cubic centimeters pre-treatment to 3.8 cubic centimeters a year after treatment. Overall, clinically significant cancer was eliminated in 80% of the study participants.
Seventy-two out of 111 men, or 65%, had no evidence of any cancer at biopsy after one year. Blood levels of prostate-specific antigen (PSA), a marker of prostate cancer, fell by a median of 95%. There were low rates of severe toxicity and no bowel complications.
“We saw very good results in the patients, with a dramatic reduction of over 90 percent in prostate volume and low rates of impotence with almost no incontinence,” Dr. Raman said.
Approved for clinical use in Europe, TULSA has just received FDA 510(k) clearance for prostate tissue ablation in the United States. Assuming follow-up studies support the preliminary results, the technique could develop into an important tool for treating both prostate cancer and benign prostatic hyperplasia, or enlargement of the prostate.
“There are two very unique things about this system,” Dr. Raman said. “First, you can control with much more finesse where you're going to treat, preserving continence and sexual function. Second, you can do this for both diffuse and localized prostate cancer and benign diseases, including benign hyperplasia.”
TULSA also has the benefit of allowing further treatment if needed, Dr. Raman said. If it fails, then the procedure can be repeated, and more aggressive invasive approaches like surgery and radiation therapy can still be used. Alternatively, TULSA may enable noninvasive treatment for localized radiation failure.
The study also supports the use of MRI for post-treatment monitoring of patients who undergo TULSA. MRI at one year after treatment had a negative predictive value of 93 to 96% for detecting residual cancer, meaning it was very accurate for ruling out disease recurrence in patients.
###
Co-authors are Aytekin Oto, M.D., Katarzyna J. Macura, M.D., Ph.D., Sandeep S. Arora, M.B.B.S., Temel Tirkes, M.D., Jurgen J. Futterer, M.D., Ph.D., Daniel N. Costa, M.D., David Bonekamp, M.D., Ph.D., Masoom A. Haider, M.D., Derek W. Cool, M.D., Ph.D., Carlos Nicolau, M.D., Thorsten Persigehl, M.D., Kiran R. Nandalur, M.D., Robert Staruch, Mathieu Burtnyk, Dipl.Phys., Marc Serrallach, M.D., Gregory Zagaja, M.D., Gencay Hatiboglu, M.D., James D. Relle, M.D., Allan Pantuck, M.D., Yair Lotan, M.D., Axel Heidenreich, M.D., Michiel Sedelaar, M.D., Ph.D., Joseph Chin, M.D., Michael Koch, M.D., Christian Pavlovich, M.D., David Penson, M.D., Laurence Klotz, M.D., and Scott Eggener, M.D.
Note: Copies of RSNA 2019 news releases and electronic images will be available online at RSNA.org/press19 beginning Monday, Nov. 25.
RSNA is an association of over 53,400 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
Editor's note: The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting.
For patient-friendly information on prostate cancer and enlargement of the prostate, visit RadiologyInfo.org.
Media Contact
All latest news from the category: Medical Engineering
The development of medical equipment, products and technical procedures is characterized by high research and development costs in a variety of fields related to the study of human medicine.
innovations-report provides informative and stimulating reports and articles on topics ranging from imaging processes, cell and tissue techniques, optical techniques, implants, orthopedic aids, clinical and medical office equipment, dialysis systems and x-ray/radiation monitoring devices to endoscopy, ultrasound, surgical techniques, and dental materials.
Newest articles

A ‘language’ for ML models to predict nanopore properties
A large number of 2D materials like graphene can have nanopores – small holes formed by missing atoms through which foreign substances can pass. The properties of these nanopores dictate many…

Clinically validated, wearable ultrasound patch
… for continuous blood pressure monitoring. A team of researchers at the University of California San Diego has developed a new and improved wearable ultrasound patch for continuous and noninvasive…

A new puzzle piece for string theory research
Dr. Ksenia Fedosova from the Cluster of Excellence Mathematics Münster, along with an international research team, has proven a conjecture in string theory that physicists had proposed regarding certain equations….



