Gene-editing alternative corrects Duchenne muscular dystrophy
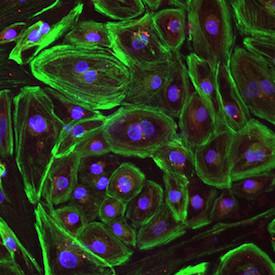
Image shows heart muscle that is missing the dystrophin molecule. Credit: UT Southwestern
The UT Southwestern group had previously used CRISPR-Cas9, the original gene-editing system, to correct the Duchenne defect in a mouse model of the disease and in human cells. In the current work, they used a new variation of the gene-editing system to repair the defect in both a mouse model and in human cells.
“We took patient-derived cells that had the most common mutation responsible for Duchenne muscular dystrophy and we corrected them in vitro to restore production of the missing dystrophin protein in the cells. This work provides us with a promising new tool in the CRISPR toolbox,” said author Dr. Eric Olson, Chairman of Molecular Biology, Co-Director of the UT Southwestern Wellstone Muscular Dystrophy Cooperative Research Center, and Director of the Hamon Center for Regenerative Science and Medicine.
The research appears in the journal Science Advances.
CRISPR-Cpf1 differs from CRISPR-Cas9 in a number of key ways. Cpf1 is much smaller than the Cas9 enzyme, which makes it easier to package inside a virus and therefore easier to deliver to muscle cells.
It also recognizes a different sequence of DNA than Cas9 does, which provides greater flexibility in terms of use. “There will be some genes that may be difficult to edit with Cas9 but may be easier to modify with Cpf1, or vice versa. The two proteins have different biochemical properties and recognize different DNA sequences, so these properties create more options for gene-editing,” said Dr. Olson, who holds the Pogue Distinguished Chair in Research on Cardiac Birth Defects, the Robert A. Welch Distinguished Chair in Science, and the Annie and Willie Nelson Professorship in Stem Cell Research.
- CRISPR/Cas9 gene editing for Duchenne MD
- UT Southwestern Wellstone Muscular Dystrophy Cooperative Research Center
- Hamon Center for Regenerative Science and Medicine.
- Olson Laboratory
“By either skipping a mutation region or precisely repairing a mutation in the gene, CRISPR-Cpf1-mediated genome editing not only corrects Duchenne muscular dystrophy mutations but also improves muscle contractility and strength,” said co-author Dr. Rhonda Bassel-Duby, Professor of Molecular Biology and Associate Director of the Hamon Center for Regenerative Science and Medicine.
Duchenne muscular dystrophy is caused by a mutation to one of the longest genes in the body. When there is a DNA error in the dystrophin gene, the body doesn't make the protein dystrophin, which serves as a sort of shock absorber for the muscle fiber. Since there are numerous places in the dystrophin gene where a mutation can occur, flexibility for gene-editing treatment is crucial.
Duchenne occurs in about 1 in every 5,000 boys, according to the Centers for Disease Control and Prevention. Duchenne muscular dystrophy is a progressive disease affecting both muscle used for movement and heart muscle, with patients typically succumbing before age 30 due to heart failure.
“CRISPR-Cpf1 gene-editing can be applied to a vast number of mutations in the dystrophin gene. Our goal is to permanently correct the underlying genetic causes of this terrible disease, and this research brings us closer to realizing that end,” Dr. Olson said.
“CRISPR-Cpf1 differs from CRISPR-Cas9 in a number of key ways, including being easier to deliver to muscle cells, said Yu Zhang, a graduate student in Dr. Olson's lab and the first author of this study.
###
Other UT Southwestern researchers who contributed to this work are Dr. Hui Li, research scientist; John R. McAnally, research scientist; Dr. Kedryn Baskin, postdoctoral researcher; and John M. Shelton, senior research scientist.
This work was supported by grants from the National Institutes of Health (NIH), a Paul D. Wellstone Muscular Dystrophy Cooperative Research Centers grant, and a Robert A. Welch Foundation grant.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution's faculty has received six Nobel Prizes, and includes 22 members of the National Academy of Sciences, 18 members of the National Academy of Medicine, and 14 Howard Hughes Medical Institute Investigators. The faculty of more than 2,700 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in about 80 specialties to more than 100,000 hospitalized patients, 600,000 emergency room cases, and oversee approximately 2.2 million outpatient visits a year.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

NASA: Mystery of life’s handedness deepens
The mystery of why life uses molecules with specific orientations has deepened with a NASA-funded discovery that RNA — a key molecule thought to have potentially held the instructions for…

What are the effects of historic lithium mining on water quality?
Study reveals low levels of common contaminants but high levels of other elements in waters associated with an abandoned lithium mine. Lithium ore and mining waste from a historic lithium…

Quantum-inspired design boosts efficiency of heat-to-electricity conversion
Rice engineers take unconventional route to improving thermophotovoltaic systems. Researchers at Rice University have found a new way to improve a key element of thermophotovoltaic (TPV) systems, which convert heat…



