How liver metastases can be stopped
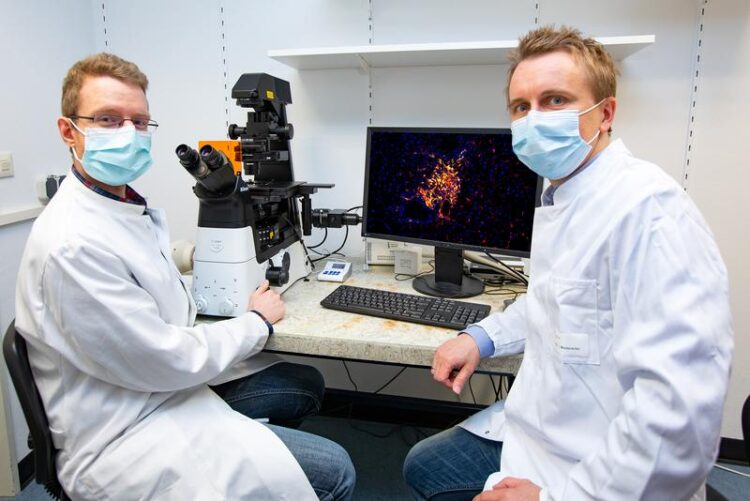
PD Dr. Ingmar Mederacke (right) and PhD student Florian Hamberger in front of a fluorescence microscope image of a metastasis with cancer-associated fibroblasts originating from hepatic stellate cells.
Copyright: Karin Kaiser / MHH
Research team investigates role of connective tissue cells in tumour environment.
Every year, more than 220,000 people die of cancer in Germany – and the number is rising. About 90 percent of these deaths are caused by metastases. These are metastases that have formed from cells of the original tumour (primary tumour). A particularly large number of metastases develop and grow in the liver. As the central organ of metabolism, it provides fertile ground for secondary tumours with an abundance of growth factors and nutrients.
An important role within this tumour microenvironment is played by connective tissue cells, the so-called cancer associated fibroblasts (CAF). A research team led by PD Dr. Ingmar Mederacke, senior physician at the Department of Gastroenterology, Hepatology and Endocrinology at Hannover Medical School (MHH), together with scientists from Columbia University in the USA, has investigated whether these cells promote or inhibit the formation of metastases and which mechanisms are responsible for this. The results have been published in the scientific journal The Journal of Clinical Investigation.
Collagen keeps tumour in check
The scientists were first able to show that the CAF cells in the liver metastases of the different tumour types originate for the most part from hepatic stellate cells, an important cell type for the scarring of the liver in liver cirrhosis. In addition, the number of fibroblasts in the respective metastases depends on the primary tumour. “In the case of skin and breast cancer, rather few CAF cells develop in the liver metastases in the models we used, whereas many do in the case of intestinal, pancreatic and bile duct tumours,” says Dr Mederacke.
The scientists studied different types of metastases in cell culture and in the mouse model. They found that the stellate cells have a dual function and can both inhibit and promote tumour growth. They were able to show that the CAFs secrete messenger substances that make the metastases grow. But there is also an antagonist. In cancers that produce many CAF cells, the secondary tumours are literally enveloped by collagen-containing connective tissue. The fibre-forming collagen ensures that the envelope scars, fibrosis tissue develops and the growth of the metastases is restricted. “The collagen apparently keeps tumour development in check mechanically,” says the gastroenterologist. “These two mechanisms explain the two opposing influences of connective tissue cells in cancer development.”
New treatment option in cancer therapy
This finding can be used therapeutically: If the research team reduced the number of hepatic stellate cells or their CAF progeny cells in the tumour microenvironment, but not the collagen, the growth of metastases decreased. However, this effect only works for metastases from tumour types where many cancer-associated fibroblasts form. Since the majority of secondary tumours cannot be surgically removed, CAF cells represent a possible therapeutic target in cancer treatment in such cases.
A key advantage here is their genetic stability – unlike cancer cells, which are always changing and can thus repeatedly develop resistance to chemotherapeutic agents, for example, the mechanisms in CAFs remain the same. “By switching off the tumour-promoting messenger substances and at the same time maintaining the collagen production of the CAF cells in the microenvironment, we can virtually flip the switch to tumour inhibition and thus open up a new treatment option for cancer metastases in the liver,” says Dr. Mederacke.
SERVICE:
For further information, please contact PD Dr. Ingmar Mederacke, mederacke.ingmar@mh-hannover.de, phone (0511) 532-6619.
The original paper “Tumour restriction by type I collagen opposes tumour-promoting effects of cancer-associated fibroblasts” can be found here:
https://www.jci.org/articles/view/146987/pdf
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Innovative 3D printed scaffolds offer new hope for bone healing
Researchers at the Institute for Bioengineering of Catalonia have developed novel 3D printed PLA-CaP scaffolds that promote blood vessel formation, ensuring better healing and regeneration of bone tissue. Bone is…

The surprising role of gut infection in Alzheimer’s disease
ASU- and Banner Alzheimer’s Institute-led study implicates link between a common virus and the disease, which travels from the gut to the brain and may be a target for antiviral…

Molecular gardening: New enzymes discovered for protein modification pruning
How deubiquitinases USP53 and USP54 cleave long polyubiquitin chains and how the former is linked to liver disease in children. Deubiquitinases (DUBs) are enzymes used by cells to trim protein…



