Microfluidic device captures, allows analysis of tumor-specific extracellular vesicles
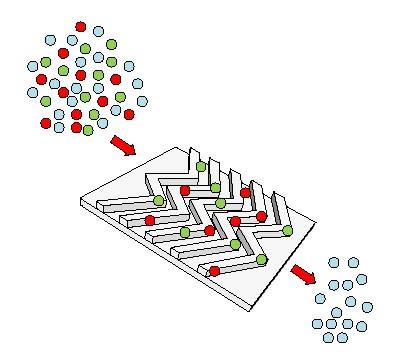
Schematic image showing how the antibody-coated surfaces of the EVHB-Chip capture red- and green-labeled tumor-specific extracellular vesicles from patient serum or plasma. Credit: Eduardo Reátegui, PhD, Center for Engineering in Medicine, Massachusetts General Hospital Usage restricted to coverage of the paper described in this release.
A new microfluidic device developed by investigators at Massachusetts General Hospital (MGH) may help realize the potential of tumor-derived extracellular vesicles (EVs) – tiny lipid particles that carry molecules through the bloodstream – as biomarkers that could monitor a tumor's response to therapy and provide detailed information to guide treatment choice.
In their report published earlier this year in Nature Communications, the team from the MGH Center for Engineering in Medicine (MGH-CEM) describes how EVs captured from serum or plasma samples of patients with the dangerous brain tumor glioblastoma multiforme (GBM) provided detailed, tumor-specific genetic and molecular information.
“Glioblastoma is a highly fatal disease with few treatment options,” says senior author Shannon Stott, PhD, of the MGH Cancer Center and the BioMEMS Resource Center in the MGH-CEM. “Due to the tumor's location, it has been challenging to get dynamic, real-time molecular information, which limits the ability to determine tumor progression and to match patients with the most promising new therapies. Our device's ability to sort tumor-specific EVs out from the billions of EVs carried through the bloodstream may lead to the development of much-needed diagnostic and monitoring tools for this and other hard-to-treat cancers.”
Previous technologies designed to isolate EVs were limited in their ability to distinguish tumor EVs from those carrying molecules from non-malignant cells. More specific approaches using tumor-specific antibodies were time-consuming and cumbersome or did not capture sufficient numbers of tumor-specific EVs from a sample.
Other “liquid biopsy” technologies designed to capture tumor cells and molecules – such as several circulating tumor cell (CTC)-isolating devices developed by member of the MGH team – may be limited in their ability to monitor brain tumors throughout treatment. Since these potential biomarkers may not consistently pass through the blood brain barrier, their presence at the time a blood sample is drawn may be limited.
Stott's team combined features of the CTC-detecting HB-Chip, which she helped to develop, with features specific to the capture of EVs. The surfaces through which a sample is passed are optimized to the physical properties of EVs – which are thousands of times smaller than cells – and contain a “cocktail” of antibodies against proteins highly expressed on GBM cells. The team also identified factors that increased the number of tumor-specific EVs captured from a sample and developed methods for releasing EVs from the device while preserving their contents for detailed analysis. Taking this approach, their device can isolate as few as 100 nanometer-sized vesicles in a one-microliter droplet of plasma.
Using the new device, dubbed the EVHB-Chip, the researchers analyzed serum or plasma samples from 13 patients with GBM and 6 control samples from healthy donors. The EVHB-Chip isolated tumor-specific EVs from all 13 patients, and identified the EGFRvIII mutation in 5 of 6 patients tested for that mutation. The captured EVs also identified genes present in the four characteristic subtypes of GBM and revealed the upregulation of more than 50 cancer-associated genes, some not previously observed in GBM EVs.
An assistant professor of Medicine at Harvard Medical School, Stott notes that the great specificity and sensitivity of the EVHB-Chip allow the use of relatively small blood samples, which would be particularly beneficial for pediatric patients for whom other blood biopsy approaches are not always feasible. The flexibility of the device should allow it to be useful for many types of cancer and, since all cells release EVs into the circulation, for other conditions including infectious diseases, autoimmune diseases, cardiac events and neurodegenerative disorders. Simultaneous investigations of biomarkers provided by EVs, CTCs and circulating DNA should help determine which can be most informative for specific patients and stages of treatment.
Stott notes that the EVHB-Chip was designed to be a low-cost, easy to use device with the hope of rapid translation to the clinic. “We are excited by this early-stage data, and we look forward to scaling the technology and increasing the number of patient samples analyzed. Specifically, we are interested in exploring how these vesicles change over time in response to treatment, and we see our blood-based assay as an ideal way to explore this in brain tumor patients,” she says.
###
The co-lead authors of the Nature Communications report are Eduardo Reátegui, PhD, of the MGH-CEM and Kristan van der Vos, PhD, and Charles Lai, PhD, MGH Neurodiscovery Center. Additional co-authors are Mahnaz Zeinali, Berent Aldikacti, Frederick Floyd Jr, Aimal Khankhel, and Mehmet Toner, PhD; MGH-CEM; Nadia Atai, PhD, Leonora Balaj, PhD, and Xandra Breakefield, PhD, MGH Neurodiscovery Center; Brian V. Nahed, MD, and Bob Carter, MD, PhD, MGH Neurosurgery and MGH Cancer Center; Vishal Thapar, Lecia Sequist, MD, and David Ting, MD, MGH Cancer Center; and Fred Hochberg, University of California at San Diego. The study was supported by National Institutes of Health grants CA069246, U19 CA179563, EB008047 and P41 EB002503-11 and grants from Voices Against Brain Cancer, the Wang Pediatric Brain Tumor Collaborative and the Canadian Institute of Health Research. The MGH has filed a patent application for the work described in this paper.
Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH Research Institute conducts the largest hospital-based research program in the nation, with an annual research budget of more than $900 million and major research centers in HIV/AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, genomic medicine, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, photomedicine and transplantation biology. The MGH topped the 2015 Nature Index list of health care organizations publishing in leading scientific journals and earned the prestigious 2015 Foster G. McGaw Prize for Excellence in Community Service. In August 2017 the MGH was once again named to the Honor Roll in the U.S. News & World Report list of “America's Best Hospitals.”
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

NASA: Mystery of life’s handedness deepens
The mystery of why life uses molecules with specific orientations has deepened with a NASA-funded discovery that RNA — a key molecule thought to have potentially held the instructions for…

What are the effects of historic lithium mining on water quality?
Study reveals low levels of common contaminants but high levels of other elements in waters associated with an abandoned lithium mine. Lithium ore and mining waste from a historic lithium…

Quantum-inspired design boosts efficiency of heat-to-electricity conversion
Rice engineers take unconventional route to improving thermophotovoltaic systems. Researchers at Rice University have found a new way to improve a key element of thermophotovoltaic (TPV) systems, which convert heat…



