Monitoring the heart's mitochondria to predict cardiac arrest?
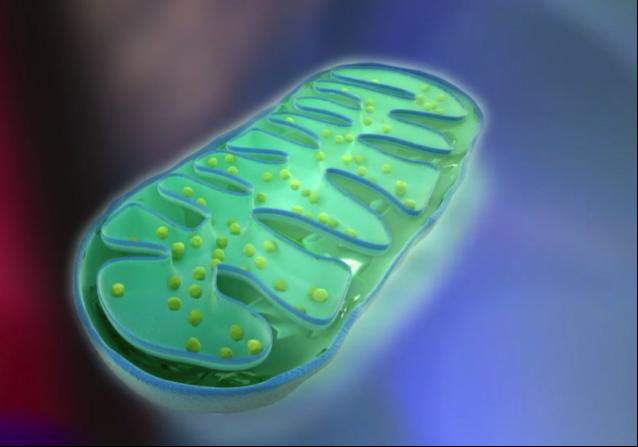
A mitochondrion Credit: Dr. John Kheir, Boston Children's Hospital & Shutterstock
A new device can assess in real time whether the body's tissues are receiving enough oxygen and, placed on the heart, can predict cardiac arrest in critically ill heart patients, report researchers at Boston Children's Hospital and scientists from Cambridge device maker Pendar Technologies. Their study, conducted in animal models, is the cover article in today's issue of Science Translational Medicine.
“With current technologies, we cannot predict when a patient's heart will stop,” says John Kheir, MD of Boston Children's Heart Center, who co-led the study. “We can examine heart function on the echocardiogram and measure blood pressure, but until the last second, the heart can compensate quite well for low oxygen conditions. Once cardiac arrest occurs, its consequences can be life-long, even when patients recover.”
The device uses a technology called resonance Raman spectroscopy to measure whether enough oxygen is reaching the mitochondria, the organelles that provide cells with energy. In critically ill patients with compromised circulation or breathing, oxygen delivery is often impaired, making it hard for mitochondria to do their job. This is especially a problem for the heart, which has constant high energy needs.
The current standard for measuring tissue oxygenation, known as mixed venous saturation (SvO2), requires repeated blood draws, adding extra risk in critically ill patients. More importantly, SvO2 cannot tell whether oxygen supply is sufficient to meet the dynamic demands of heart muscle.
“We wanted to create an organ-specific, continuous, reliable readout of how adequately mitochondria are being fed oxygen,” says Kheir. “This is the first demonstration of a device that can monitor mitochondria in living tissues to predict impending organ failure.”
Using light to monitor mitochondria
This technology is the product of a collaboration between the Translational Research Lab in Boston Children's Heart Center, co-led by Kheir and Brian Polizzotti, PhD, and Pendar Technologies (Cambridge, Mass.). “At the bedside, we saw patients who had a limitation to coronary blood flow, and wanted a device that could provide an early warning sign,” Kheir says.
The team created a metric they call 3RMR that uses light readings generated by resonance Raman spectroscopy to quantify oxygenation and mitochondrial function in real time.
When a cell's oxygen levels are too low, its energy balance changes. Electrons start to build up in certain cellular proteins — hemoglobin, myoglobin and mitochondrial cytochromes. This energy shift reduces or shuts down mitochondrial energy production and can also trigger cell death. All of this sets the stage for organ injury or dysfunction and, in the worst case, cardiac arrest, says Kheir.
Resonance Raman spectroscopy quantifies the fraction of mitochondrial proteins with electrons on them based on how light is scattered when a laser is shined on them. Under low-oxygen conditions, the gain in electrons causes these molecules to distort and, as a result, their spectrum changes.
“This system tells us how satisfied the mitochondria are with their oxygen supply,” Kheir explains.
The team used a precise laser and a complex algorithm to distill the information in real time.
“Distinguishing mitochondrial signals from other biological signals with accuracy and speed was the most significant scientific advance here,” says Pendar CEO Daryoosh Vakhshoori, PhD, who oversaw the engineering aspect of the project.
Predicting cardiac arrest
Joshua Salvin, MD, MPH and Dorothy Perry, MBChB of the Heart Center, the study's co-first authors, tested the device in rat models. They found that reduced oxygenation of the heart corresponded with elevations in 3RMR, regardless of the cause of reduced oxygen delivery. Elevations of more than 40 percent, measured after 10 minutes of low-oxygen conditions, predicted reduced heart contractility and subsequent cardiac arrest with 97 percent specificity and 100 percent sensitivity, outperforming all other measurement techniques.
The team further tested the device during simulated congenital heart surgery in a pig model. They were able to measure how satisfied the heart muscle was with its oxygen supply, something that cannot currently be done.
“Our likely first application of this device will be to monitor oxygen delivery during and after heart surgery,” says Kheir. The current probe is the size of a pen, but eventually, the team would like to develop a smaller probe that could be left inside the chest, so patients could be monitored in the ICU during highest-risk times.
Future applications
Kheir and colleagues also believe the technology could be used to monitor tissue viability in other operations in which tissues and organs are exposed. Potential applications might include monitoring organs intended for transplantation and detection of dangerously reduced blood flow in limbs.
“I think there would be many surgical uses,” says Vakhshoori, co-corresponding author on the study. “There really is no technology currently that can assess, in real time, whether oxygen delivery to a tissue is adequate at the level of the mitochondrion.”
Kheir also thinks the tool could be helpful in cancer research, since mitochondrial function is central to cancer biology.
The team's goal is to seek FDA approval and commercialize a bedside monitor of mitochondrial oxygenation. In the meantime, Kheir and colleagues plan to seek approval to test the device to monitor heart patients.
###
Other coauthors on the study were Padraic Romfh, Peili Chen and Kalyani Krishnamurthy of Pendar Technologies; Lindsay M. Thomson and Brian D. Polizzotti of Boston Children's and Francis X. McGowan of the Children's Hospital of Philadelphia. Pendar Technologies holds an exclusive license to U.S. patent 7,113,814 entitled “Tissue Interrogation Spectroscopy.” The study was funded by AHA IRG (14IRG18430027), DOD ATTDA (W81XWH-15-1-0544), DOD BRA (W81XWH-11-2-0041), Smith Family President's Innovator Award and Hess Family Philanthropic Fund.?
About Boston Children's Hospital
Boston Children's Hospital, the primary pediatric teaching affiliate of Harvard Medical School, is home to the world's largest research enterprise based at a pediatric medical center. Its discoveries have benefited both children and adults since 1869. Today, more than 2,630 scientists, including nine members of the National Academy of Sciences, 14 members of the National Academy of Medicine and 11 Howard Hughes Medical Investigators comprise Boston Children's research community. Founded as a 20-bed hospital for children, Boston Children's is now a 415-bed comprehensive center for pediatric and adolescent health care. For more, visit our Vector and Thriving blogs and follow us on social media @BostonChildrens, @BCH_Innovation, Facebook and YouTube.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Can lab-grown neurons exhibit plasticity?
“Neurons that fire together, wire together” describes the neural plasticity seen in human brains, but neurons grown in a dish don’t seem to follow these rules. Neurons that are cultured…

Unlocking the journey of gold through magmatic fluids
By studying sulphur in magmatic fluids at extreme pressures and temperatures, a UNIGE team is revolutionising our understanding of gold transport and ore deposit formation. When one tectonic plate sinks…

3D concrete printing method that captures carbon dioxide
Scientists at Nanyang Technological University, Singapore (NTU Singapore) have developed a 3D concrete printing method that captures carbon, demonstrating a new pathway to reduce the environmental impact of the construction…



