New approach developed to predict response of immunotherapies in lung cancer
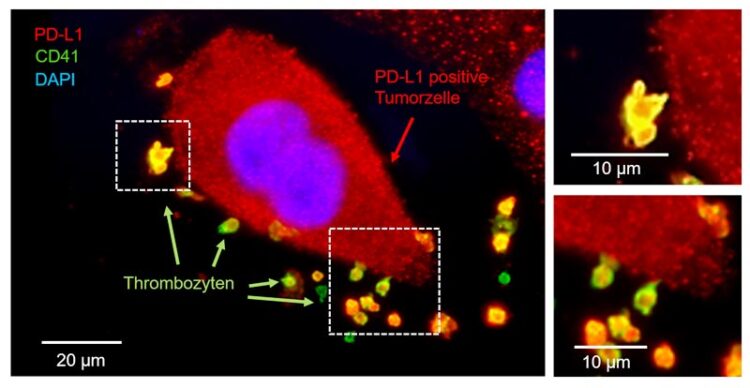
Platelets interact with a lung tumor cell, taking up the molecule PD-L1. © University Hospital Tübingen
New methodology at the University Hospital of Tübingen harnesses the function of platelets.
Lung cancer is one of the most frequent and deadly malignancies in the world, with 1.8 million fatalities per year. In Germany alone, the disease claimed the lives of about 45,000 individuals in 2019. Treatment options for lung cancers have improved in recent years thanks to novel cancer medicines such so-called “checkpoint inhibitor-based” immunotherapies. These therapies work by inhibiting certain signaling pathways in the immune system, triggering a defense response against tumor cells. These checkpoints are based on so-called surface receptors and molecules, such as PD-1 or PD-L1. Through a specific antibody-mediated inhibition of these molecules, the immune system recognizes the tumor as an enemy and attacks it. Thanks to this therapy concept, a containment of the cancer can be achieved in about 20 percent of all lung tumor patients.
“Despite this success, there is still no reliable method to predict which patients will respond to immunotherapy,” explains Dr. Clemens Hinterleitner. Not every patient responds equally well to the therapy, undesirable side effects can occur, and immunotherapy is extremely cost-intensive. This underlines the importance and potential of the newly developed method. “We found that blood platelets that come into contact with the tumor cell, take up the molecule PD-L1. Our study was able to show that the number of PD-L1-loaded platelets is a very good indicator of whether immunotherapy with PD-1 or PD-L1 blocking antibodies in lung tumors is promising or not,” says Dr. Hinterleitner.
One of the main criteria for successful immunotherapy using PD-1 or PD-L1 blocking antibodies is the presence of PD-L1 on the tumor cell. Before immunotherapy is even considered, blood is drawn from patients with lung tumors. The laboratory next assesses whether there are enough PD-L1 molecules on the platelet surface to further assess whether cancer immunotherapy is a viable option in this circumstance.
“Platelets circulate through our bloodstream thousands of times a day and inevitably come into contact with any tumor cells that may be present. By taking up the molecule PD-L1, they are particularly well suited as a biomarker that can more precisely predict the response towards a checkpoint inhibitor therapy,” adds Prof. Dr. Lars Zender. Although there are already methods to predict a response of immunotherapy, such as the so-called immunohistochemical staining. Here, a biopsy of the tumor is taken and staining of cell or tissue structures is performed with dyes coupled to antibodies. A very specific property of the tissue then triggers an antigen-antibody response. “The problem with studies on biopsy material, however, is that tumors are very heterogeneous and that a single biopsy does not adequately reflect the totality of the tumor. Compared to existing immunohistochemical methods, our methodology using platelets has a much better predictability,” Prof. Zender explains the difference.
With the iFIT Cluster of Excellence, the only cluster of excellence on oncology research in Germany, and the appointment of Tübingen as a new site in the National Center for Tumor Diseases (NCT), optimal conditions are available to further investigate these promising findings and validate them in a multicenter study.
Wissenschaftliche Ansprechpartner:
University Hospital Tübingen
Medical Oncology & Pneumology (Internal Medicine VIII)
Medical Director & Chair
Professor Dr. Lars Zender
Otfried-Müller-Straße 14, 72076 Tübingen
Tel. +49 7071 29-83675
E-Mail lars.zender@med.uni-tuebingen.de
University Hospital Tübingen
Medical Oncology & Pneumology (Internal Medicine VIII)
Specialist in internal medicine and hematology and oncology
Dr. Clemens Hinterleitner
Otfried-Müller-Straße 14, 72076 Tübingen
E-Mail clemens.hinterleitner@med.uni-tuebingen.de
Originalpublikation:
Original title of the publication: Hinterleitner, C., Strähle, J., Malenke, E. et al. Platelet PD-L1 reflects collective intratumoral PD-L1 expression and predicts immunotherapy response in non-small cell lung cancer. Nat Commun 12, 7005 (2021).
DOI: 10.1038/s41467-021-27303-7
The publication is available at the following link: https://www.nature.com/articles/s41467-021-27303-7
https://www.medizin.uni-tuebingen.de/en-de/das-klinikum/pressemeldungen/459?press_str=
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Tackling Life-Threatening Fungal Infections Using RNA Modifications
Importance of RNA modifications for the development of resistance in fungi raises hope for more effective treatment of fungal infections. An often-overlooked mechanism of gene regulation may be involved in…

Unraveling Aphasia: Global Study Breaks Down Patients’ Struggle with Verb Tenses
An international team of researchers, including scientists from the HSE Centre for Language and Brain, has identified the causes of impairments in expressing grammatical tense in people with aphasia. They discovered…

Facing the Storm: A Prepped Up Future Against Extreme Climatic and Weather Changes
From the persistent droughts of southern Africa and Central America in the early part of the year to the more recent devastating extreme rainfall in Spain and the deadly Hurricane…



