Researchers develop new approach for vanquishing superbugs
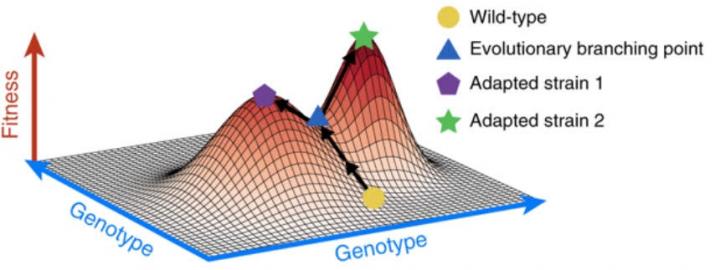
Researchers developed a new way to identify second-line antibiotics that may be effective in killing germs already resistant to a first-line antibiotic -- potentially helping overcome antibiotic resistance. This new research provides an approach clinicians could consult when deciding which antibiotic treatment courses will be most effective for patients. Credit: Jacob Scott, MD, DPhil
A scientific team from Case Western Reserve University School of Medicine and Cleveland Clinic has developed a new way to identify second-line antibiotics that may be effective in killing germs already resistant to a first-line antibiotic – potentially helping overcome antibiotic resistance.
This new research provides an approach clinicians could consult when deciding which antibiotic treatment courses will be most effective for patients.
The method is based on a mathematical model created by Jacob Scott, MD, DPhil, principal investigator and associate staff member at Cleveland Clinic, and a clinical assistant professor at the medical school, and colleagues.
In a recent Nature Communications study, the researchers tested implications of the model in 60 different scenarios with a large panel of currently available antibiotics against E. coli strains that had evolved resistance to the widely-used antibiotic cefotaxime.
By using numerous evolution experiments, coupled with whole genome sequencing, they found drugs with a higher likelihood of being effective after resistance initially emerged to cefotaxime.
Once researchers expand these findings to a larger panel of initial therapies, physicians should be able to pinpoint with better accuracy which follow-up antibiotics are likely to work against resistant superbugs – overcoming a shortfall in current approaches.
Antibiotic resistance occurs when invading germs such as bacteria and fungi evolve the ability to outmaneuver antibiotics that used to wipe them out. Instead of being destroyed, the resulting superbugs thrive, sickening – and potentially killing – patients who, in the past, would have been healed by an effective medication.
While known for decades, the problem is worsening as a result of over-use of antibiotics in food and when treating patients. Each year in the U.S., at least two million people are infected with antibiotic-resistant bacteria, and at least 23,000 people die as a result.
The solution seems obvious: create new medicines to outwit the germs or use different antibiotics to see if they work instead. But bringing an average drug to market is expensive: $2.7 billion, according to a widely-used projection by the Tufts Center for the Study of Drug Development.
And only a few new antibiotics have been developed over the past 30 years. There's another problem: “While new antibiotics may bring short- and medium-term relief, germs will eventually develop ways to outfox them,” says Scott, who is also a physician-scientist in the department of Translational Hematology and Oncology Research at Cleveland Clinic Lerner Research Institute.
“Then we're back to where we started. That's just how evolution works. As the Red Queen tells Alice in Through the Looking Glass, 'It takes all the running you can do to keep in the same place.'”
The study's lead experimentalist, Robert A. Bonomo, MD, professor of medicine, pharmacology, molecular biology and microbiology at Case Western Reserve, and chief of medical service at the Louis Stokes Cleveland Department of Veterans Affairs Medical Center, makes it clear that he and his co-authors are not opposed to developing new medicines: “After all, that's what's been done in the past.
For example, tetracycline and erythromycin were developed decades ago when resistance surfaced against penicillin, and they've both proven very effective. And while germs will develop resistance to new medications, it may take years to do so. But correctly using existing medications can bring much quicker relief to patients and help keep health care costs contained.”
In the new study, the authors administered a panel of different antibiotics to 60 E. coli strains that had been made resistant to cefotaxime. They then assessed whether the E. coli were killed off at higher or lower rates than E. coli that had not been made resistant to cefotaxime.
By using a much larger number of trials than is typical, the researchers overcame the problem of skewed results, which can lead clinicians to infer that a replacement antibiotic is more or less effective than it actually is when given to patients.
“Using a large number of what we term 'evolutionary replicates' explicitly accounts for the inherent randomness of evolution,” said Bonomo. “If you only carry out a handful of tests, you are likely to miss the complexity of the evolutionary response of a bug to a second antibiotic.”
In the case of ticarcillin, one of the antibiotics tested in the study, the researchers found that in only seven of the 60 replicates (11 percent of the time) did the resistant E. coli die at a higher rate compared pair-wise to E. coli not resistant to cefotaxime.
“This means that 89 percent of the time, this would be a bad second drug to give when dealing with cefotaxime-resistant E. coli,” said the study's lead theorist, Daniel Nichol, DPhil, who undertook this research during his doctoral studies in the Department of Computer Science at the University of Oxford.
The authors found similar low rates of effectiveness for other drugs tested in the same drug family. “These findings serve as a cautionary warning that we may be inadvertently promoting resistance by prescribing follow-through drugs based on too few trials of their effectiveness.”
“This paper is a first step in establishing a repository of findings that a clinician could consult in trying to determine how to deal with patients confronting CEF-resistant E. coli and eventually, other superbugs,” said Scott. “We showed that not only is the common approach of using a few trials often less effective than hoped for, it may actually increase the risk to patients by wasting valuable time and resources in combating a serious infection.”
###
Funding for the study was provided by the National Institutes of Health, National Cancer Institute, U. S. Department of Veterans Affairs, the Engineering and Physical Sciences Research Council, Cleveland Department of Veterans Affairs, and the Cleveland Geriatric Research Education and Clinical Center.
Scott, J., Bonomo, R. et al. “Antibiotic collateral sensitivity is contingent on the repeatability of evolution.” Nature Communications 10:334 (2019).
For more information about Case Western Reserve University School of Medicine, please visit: case.edu/medicine.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

First-of-its-kind study uses remote sensing to monitor plastic debris in rivers and lakes
Remote sensing creates a cost-effective solution to monitoring plastic pollution. A first-of-its-kind study from researchers at the University of Minnesota Twin Cities shows how remote sensing can help monitor and…

Laser-based artificial neuron mimics nerve cell functions at lightning speed
With a processing speed a billion times faster than nature, chip-based laser neuron could help advance AI tasks such as pattern recognition and sequence prediction. Researchers have developed a laser-based…

Optimising the processing of plastic waste
Just one look in the yellow bin reveals a colourful jumble of different types of plastic. However, the purer and more uniform plastic waste is, the easier it is to…



