Treatment of Overweight: Is Metabolically Healthy Obesity a Worthwhile Initial Goal?
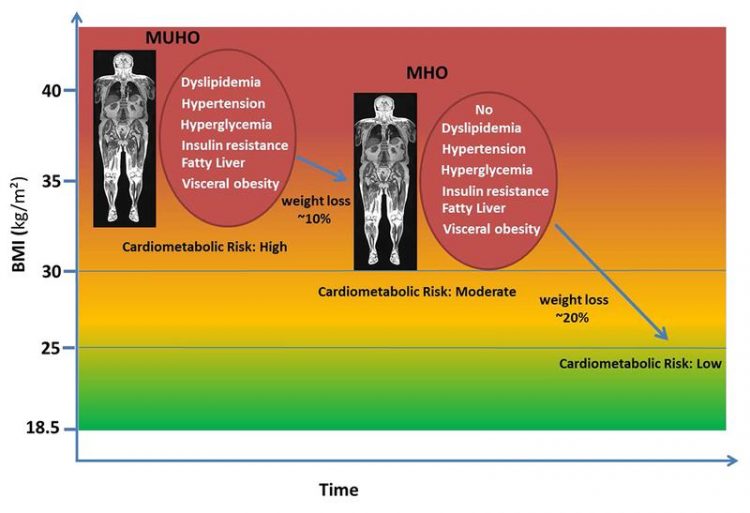
In comparison to people with metabolically abnormal obesity those with metabolically healthy obesity have 25% increased cardiometabolic risk compared to people with normal weight. Source: DZD/IDM
“Being overweight causes serious health problems. You should lose weight.” Doctors repeatedly point this out to their overweight and obese patients. Through a lifestyle intervention, the affected individuals often lose weight in the short term, but they usually fail in the long term. Furthermore, the question is whether the 5-8 per cent weight loss rate recommended by the medical associations is at all sufficient for every overweight or obese person to significantly reduce the risk of long-term severe health consequences.
At an initial weight of e.g. 120 kg and a height of 180 cm (BMI, body mass index 37.0), the BMI of the patient would thus be 34.4 after the successful weight loss. He/she would not have yet achieved the desirable BMI of 25 or less, the level at which most people are clearly protected against obesity-related illnesses.
Wouldn’t it be more meaningful to define achievable intermediate goals to reach an individual healthy weight? What parameters could describe this intermediate goal? Can smaller steps more effectively help motivate those affected to lose weight? These were the key questions in a study conducted by scientists at the Medical Clinic IV of Tübingen University Hospital / the Institute for Diabetes Research and Metabolic Diseases (IDM) of Helmholtz Zentrum München and the German Institute of Human Nutrition (DIfE) in Potsdam.
Both are partners in the German Center for Diabetes Research (DZD). In their current study, the professors Norbert Stefan and Hans-Ulrich Häring from Tübingen and Professor Matthias Schulze from Potsdam show how the concept of metabolically healthy obesity can be integrated into the risk management of obesity therapy.
Based on their own data from the Tübingen Lifestyle Intervention Study, they show that a weight loss of more than 10 percent with an average baseline BMI of 35 is likely to be sufficient to get from “metabolically unhealthy obesity (MUHO)” to “metabolically healthy obesity (MHO)”. However, they also stress the fact that that this percentage is not enough in the long term, since the disease risk for MHO individuals is still increased by 25 percent compared to metabolically healthy people with normal weight.
In contrast: for MUHO people, who weigh just a bit more than MHO people, the risk of severe health consequences is 150 percent higher, compared to the same metabolically healthy people with normal weight.
As an important intermediate step, Stefan describes the achievement of MHO as a documented protection against obesity-related metabolic diseases: “Look at this protection as a low-hanging fruit. Although it is not easy to harvest, it is easier to achieve than to concentrate on the top fruits from the outset. “The doctor / patient communication is an important support to motivate the patient to reach and at least maintain this condition.
The topic “The paradox of metabolically healthy obesity” led by Nobert Stefan will be on the program agenda at the Diabetes Congress of the EASD (European Association for the Study of Diabetes), which will be held in Lisbon from 11 to 15 September.
* People with metabolically healthy obesity have at most only one of the following risk factors: high blood pressure (hypertension), disturbed carbohydrate metabolism (insulin resistance), lipid metabolism (dyslipidemia), abdominal obesity, hyperglycemia or fatty liver .
Original Publication:
Stefan N, Häring H-U, Schulze MB. Metabolically healthy obesity: the low-hanging fruit in obesity treatment?. Lancet Diabetes Endocrinol 2017. http://dx.doi.org/10.1016/S2213-8587(17)30292-9.
Contacts:
Prof. Dr. med. Norbert Stefan
Prof. Dr. med. Dr. h.c. Hans-Ulrich Häring
Tübingen University Hospital, Medical Clinic IV
Institute for Diabetes Research and Metabolic Diseases (IDM) of Helmholtz Zentrum München at the University of Tübingen
Otfried-Müller-Str. 10, 72076 Tübingen, Germany
Phone 1: +49 (0) 7071-2985669
Phone 2: +49 (0)7071 29-80390
Phone 3: +49 (0)7071 29-83670
norbert.stefan@med.uni-tuebingen.de
Prof. Dr. Matthias Schulze
German Institute of Human Nutrition Potsdam-Rehbrücke (DIfE)
Arthur-Scheunert-Allee 114-116, 14558 Nuthetal, Germany
Phone 1: +49 (0) 033 200 88 2434
mschulze@dife.de
Media Contact:
Birgit Niesing
German Center for Diabetes Research
Ingolstädter Landstr. 1
85764 Neuherberg
Gerrmany
Phone: +49(0)89-3187-3971
email: niesing@dzd-ev.de
The German Center for Diabetes Research (DZD) is one of six German Centers for Health Research. It brings together experts in the field of diabetes research and integrates basic research, epidemiology, and clinical applications. By adopting an innovative, integrative approach to research, the DZD aims to make a substantial contribution to the successful personalized prevention, diagnosis and treatment of diabetes mellitus. The members of the DZD are Helmholtz Zentrum München – German Research Center for Environmental Health, the German Diabetes Center (DDZ) in Düsseldorf, the German Institute of Human Nutrition (DIfE) in Potsdam-Rehbrücke, the Institute of Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, the Paul Langerhans Institute Dresden of Helmholtz Zentrum München at the Carl Gustav Carus University Hospital of TU Dresden, associated partners at the universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich, and other project partners. http://www.dzd-ev.de/en
As German Research Center for Environmental Health, Helmholtz Zentrum München pursues the goal of developing personalized medical approaches for the prevention and therapy of major common diseases such as diabetes mellitus and lung diseases. To achieve this, it investigates the interaction of genetics, environmental factors and lifestyle. The Helmholtz Zentrum München has about 2,300 staff members and is headquartered in Neuherberg in the north of Munich. Helmholtz Zentrum München is a member of the Helmholtz Association, a community of 18 scientific-technical and medical-biological research centers with a total of about 37,000 staff members. http://www.helmholtz-muenchen.de/en
Founded in 1805, Tübingen University Hospital is one of the leading centers of German university medicine. As one of 33 university hospitals in Germany, it contributes to a successful combination of top-level medicine, research, and teaching. More than 400,000 in- and outpatients from around the world benefit from this connection of science and practice each year, since the clinics, institutes, and centers unite specialists from all fields under one roof. These experts collaborate across disciplines and offer state-of-the-art research-based treatment to all patients. Here research is conducted to improve diagnostics, therapies, and prospects of recovery. Many new cutting-edge treatments are clinically tested and applied in Tübingen. Neurosciences, Oncology and Immunology, Infection Biology, Vascular Medicine and Diabetes are focus areas of research at Tübingen University Hospital, which is a reliable partner in four of the six German Centers for Health Research (DZG) created by the Federal Government. http://www.medizin.uni-tuebingen.de/en
The German Institute of Human Nutrition Potsdam-Rehbruecke (DIfE) is a member of the Leibniz Association. It investigates the causes of diet-related diseases in order to develop new strategies for prevention and therapy and to provide dietary recommendations. Its research focus includes the causes and consequences of the metabolic syndrome, which is a combination of obesity, high blood pressure, insulin resistance and lipid metabolism disorder, as well as the role of diet in healthy aging and the biological basis of food choices and eating habits. In addition, DIfE is a partner of the German Center for Diabetes Research (DZD), which was founded in 2009 and has since been funded by the BMBF. http://www.dife.de/en
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Innovative 3D printed scaffolds offer new hope for bone healing
Researchers at the Institute for Bioengineering of Catalonia have developed novel 3D printed PLA-CaP scaffolds that promote blood vessel formation, ensuring better healing and regeneration of bone tissue. Bone is…

The surprising role of gut infection in Alzheimer’s disease
ASU- and Banner Alzheimer’s Institute-led study implicates link between a common virus and the disease, which travels from the gut to the brain and may be a target for antiviral…

Molecular gardening: New enzymes discovered for protein modification pruning
How deubiquitinases USP53 and USP54 cleave long polyubiquitin chains and how the former is linked to liver disease in children. Deubiquitinases (DUBs) are enzymes used by cells to trim protein…



