CAR-T cell cancer immunotherapy gets personal
A new study performed in collaboration by David Mooney’s team at the Wyss Institute and Harvard SEAS and Catherine Wu’s team at the DFCI used these artificial antigen-presenting cell-mimicking scaffolds (APC-ms) to create personalized CAR-T cell products from patients’ T cells.
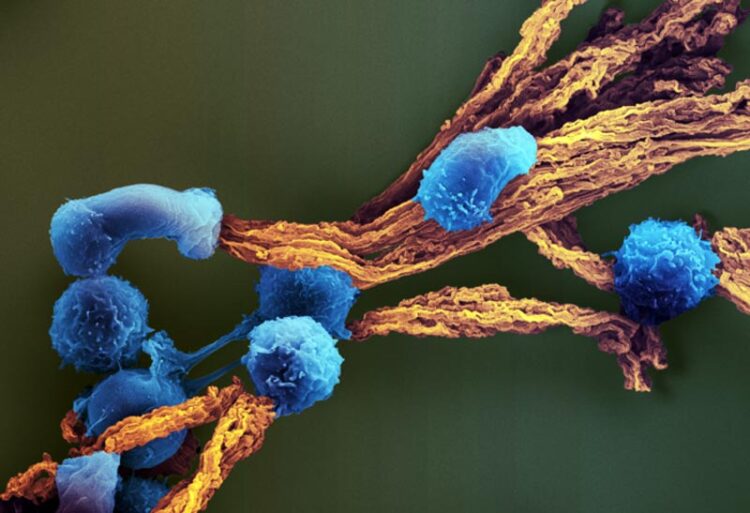
Credit: Wyss institute at Harvard University
Fine-tuning stimulation doses to deficiencies in patient-specific CAR-T cells, using artificial antigen-presenting scaffolds, enables manufacturing of more potent CAR-T cell products.
New adoptive T cell therapies — in which T cells, the immune system’s natural hunters patrolling the body for foreign adversaries, are retrieved from cancer-riddled patients, super-charged and amplified outside the body, and then infused back into the same patient — are changing the prospects of cancer patients. Since 2017, when CAR (chimeric antigen receptor)-T cells were green-lighted as the first modified therapeutic cells by the Federal Drug Administration (FDA) to treat leukemia, five similar products have since been approved and more than 20,000 people have been treated with this game-changing immunotherapy.
CAR-T cells are engineered to carry synthetic membrane-spanning receptor molecules that use their outside-facing portion to bind to antigens on cancer cells, which their inside-facing portion responds to by switching on a powerful tumor cell-destroying program. However, not all patients respond equally well to CAR-T cell therapies, and cancer immunologists have been trying to figure out what makes them work well or fail. Despite a budding understanding of differences between cancer patients’ T cells and healthy individuals’ T cells, these insights have not been taken into account in CAR-T cell manufacturing processes. All processes use a similar type of stimulation with T-cell specific agonists and general immune-stimulating cytokines to create infusible CAR-T cell products, irrespective of variations in the original T cells’ phenotype.
Now, a collaboration between bioengineers at the Wyss Institute for Biologically Inspired Engineering at Harvard University and Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) led by David Mooney, Ph.D. and cancer-immunologists at the Dana-Farber Cancer Institute (DFCI) led by Catherine Wu, M.D., Ph.D. has demonstrated that personalizing CAR-T cell stimulation during manufacturing can significantly enhance the consistency and potency of the resulting CAR-T cell products. By using artificial antigen-presenting cell mimicking scaffolds (APC-ms), the team was able to fine-tune the levels of T cell stimulation to match the phenotype of T cells obtained from leukemia patients, and significantly enhanced their ex vivo and in vivo tumor-clearing abilities. The findings are published in Nature Communications.
“We show that CAR-T cell products made from T cells derived from cancer patients are generally less functional than CAR-T cells products derived from healthy individuals,” said Founding Wyss Core Faculty member Mooney. “Matching the CAR-T cell antigen-stimulation dose to the phenotype of patients’ T cells using a precisely controllable biomaterials approach that closely mimics natural antigen presentation can significantly improve their function. This approach could further personalize CAR-T cell therapy and remove an existing inadequacy from current T cell manufacturing.” Mooney also is Robert P. Pinkas Family Professor of Bioengineering at SEAS, and a lead of the NIH-funded Immunomaterials to Improve Immunotherapy (i3) Center coordinated at the Wyss Institute. This project was conceived at the Center, and Wu is one of its Principal Investigators.
Cutting the keys for personalized CAR-T therapies
The team investigated the phenotypes of T cells that they isolated from samples obtained from patients suffering from acute lymphoblastic leukemia (ALL) and chronic lymphoblastic leukemia (CLL), as well as from healthy donors. Next, they utilized APC-ms to provide the T cells with different doses of anti-CD3/anti-CD28 antigen stimulation and thus created a CAR-T cell library. All CAR-T cell products contained in the library were then probed again for functional differences, including their ability to kill cancer cells in vitro. The researchers directly compared their approach with one that is commonly used in CAR-T cell manufacturing, which presents the same antigens on rigid magnetic beads (Dynabeads) to T cells.
A key finding was that cancer patients’ T cells were much more easily over-stimulated at antigen doses commonly used during CAR-T cell manufacturing than “healthy” T cells. This made them lose their functionality, or become more “exhausted” as immunologists say, and decreased their ability to proliferate. CAR-T cells not only need to be transformed into a functional state but also amplified by millions to be able to eliminate tumor cells and metastasis in the entire body.
“By exploring a precise, narrow range of stimulation doses made possible with APC-ms, we show that there is something like a personalized ‘sweet spot’ for patient-derived T cells that maximizes functionality and amplification, which is, on average, lower than the usual doses,” said first-author David Zhang, who is a graduate student on Mooney’s team. “The APC-ms approach functions much more naturally than Dynabeads, because highly controllable levels of T-cell signals are embedded into a lipid bilayer, which allows the CAR-T cells to push and pull at them as just as T cells usually do across the ‘immunological synapse’ between them and antigen-presenting cells when T cell stimulation is at its best.”
From in vitro studies to cell manufacturing
While the team did not observe any significant differences between CAR-T cells created from ALL and CLL patient samples, overall their approach generated more cells with high cytotoxic potential toward tumor cells, a more balanced ratio between cytotoxic CD8+ T cells and CD4+ T cells that support their function, and more memory T cells that themselves are not cytotoxic but can be activated in later responses. In a mouse in vivo study, infused CAR-T cell products created with different levels of stimulation also exhibited significantly different abilities to control CD19-expressing Burkitt’s lymphoma, with cells again stimulated at lower than usual levels during manufacturing showing the strongest potential.
“We constructed a proof-of-concept model that is based on the quantifiable relationship between the phenotype of a T cell blood sample and its CAR-T cell products, and that outputs an optimal T cell stimulation dose for personalized CAR-T cell production,” said Wu. “Given that T cell samples are always fingerprinted for important markers at the beginning of the cell manufacturing process, similar strategies could be devised to further personalize the therapy using the APC-ms approach.” Wu is the Lavine Family Chair, Preventative Cancer Therapies at DFCI, and Professor of Medicine at Harvard Medical School.
“Dave Mooney’s team in the Wyss’ Immunomaterials platform is pushing the envelope of CAR-T cell and other immunotherapies using entirely new engineering and materials-based approaches. Hopefully, this will eventually enable us to also mobilize the immune system against recalcitrant solid tumors for which no therapies exist yet. It’s also a great example of where less is more,” said Wyss Founding Director Donald Ingber, M.D., Ph.D., who is also the Judah Folkman Professor of Vascular Biology at HMS and Boston Children’s Hospital, and Hansjörg Wyss Professor of Bioinspired Engineering at the Harvard John A. Paulson School of Engineering and Applied Sciences.
Additional authors on the study are Wyss and SEAS researchers Kwasi Adu-Berchie, Siddharth Iyer, Yutong Liu, and Joshua Brockman; DFCI researcher Nicoletta Cieri, and Donna Neuberg, Sc.D., a data scientist at the DFCI and member of the i3 Center. The study was funded by the Wyss Institute at Harvard University, the Food and Drug Administration (under award #5R01FD006589), the National Cancer Institute of the NIH (under award #U54CA244726), as well as a fellowship from the Canadian Institutes of Health Research.
PRESS CONTACT
Wyss Institute for Biologically Inspired Engineering at Harvard University
Benjamin Boettner, benjamin.boettner@wyss.harvard.edu, +1 617-432-8232
###
The Wyss Institute for Biologically Inspired Engineering at Harvard University (www.wyss.harvard.edu) is a research and development engine for disruptive innovation powered by biologically-inspired engineering with visionary people at its heart. Our mission is to transform healthcare and the environment by developing ground-breaking technologies that emulate the way Nature builds and accelerate their translation into commercial products through formation of startups and corporate partnerships to bring about positive near-term impact in the world. We accomplish this by breaking down the traditional silos of academia and barriers with industry, enabling our world-leading faculty to collaborate creatively across our focus areas of diagnostics, therapeutics, medtech, and sustainability. Our consortium partners encompass the leading academic institutions and hospitals in the Boston area and throughout the world, including Harvard’s Schools of Medicine, Engineering, Arts & Sciences and Design, Beth Israel Deaconess Medical Center, Brigham and Women’s Hospital, Boston Children’s Hospital, Dana–Farber Cancer Institute, Massachusetts General Hospital, the University of Massachusetts Medical School, Spaulding Rehabilitation Hospital, Boston University, Tufts University, Charité – Universitätsmedizin Berlin, University of Zürich, and Massachusetts Institute of Technology.
The Harvard John A. Paulson School of Engineering and Applied Sciences (http://seas.harvard.edu) serves as the connector and integrator of Harvard’s teaching and research efforts in engineering, applied sciences, and technology. Through collaboration with researchers from all parts of Harvard, other universities, and corporate and foundational partners, we bring discovery and innovation directly to bear on improving human life and society.
Journal: Nature Communications
DOI: 10.1038/s41467-023-36126-7
Method of Research: Experimental study
Subject of Research: Human tissue samples
Article Title: Enhancing CAR-T cell functionality in a patient-specific manner
Article Publication Date: 31-Jan-2023
Media Contact
Benjamin Boettner
Wyss Institute for Biologically Inspired Engineering at Harvard
Benjamin.Boettner@wyss.harvard.edu
Office: 917-913-8051
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Innovative 3D printed scaffolds offer new hope for bone healing
Researchers at the Institute for Bioengineering of Catalonia have developed novel 3D printed PLA-CaP scaffolds that promote blood vessel formation, ensuring better healing and regeneration of bone tissue. Bone is…

The surprising role of gut infection in Alzheimer’s disease
ASU- and Banner Alzheimer’s Institute-led study implicates link between a common virus and the disease, which travels from the gut to the brain and may be a target for antiviral…

Molecular gardening: New enzymes discovered for protein modification pruning
How deubiquitinases USP53 and USP54 cleave long polyubiquitin chains and how the former is linked to liver disease in children. Deubiquitinases (DUBs) are enzymes used by cells to trim protein…



