PET scans help guide drug to best treat orthopaedic implant bacterial infections
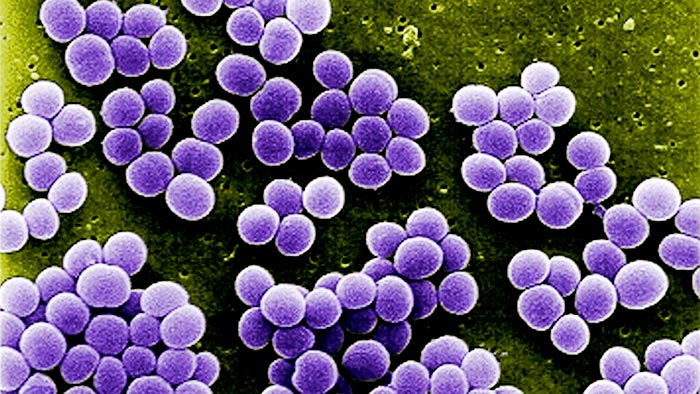
Johns Hopkins Medicine researchers have shown that PET scans can be used to “see” the movement of the drug rifampin in a living body, so that it can better treat bacterial infections — such as the Staphylococcus aureus microbes seen here — attacking orthopaedic implant-assisted bone.
Courtesy of the U.S. Centers for Disease Control and Prevention
Johns Hopkins-led imaging research helps quantify antibiotic levels, improve antibiotic action and prevent bacterial resistance.
Treating bacterial infections associated with orthopaedic implants has often been a case of too little, too late. The traditional therapy has been a combination of prolonged antibiotics, including rifampin, a 50-year-old drug that has been a staple in the global fight against tuberculosis and other bacterial diseases. However, the inability to determine how much rifampin reaches the target site can be disastrous. If not enough rifampin gets to the bacteria infesting implant-assisted bone, it not only limits the drug’s effectiveness, it can lead to development of an antibiotic-resistant strain. Once that happens, even massive doses of medication won’t help.
In a recent study published Dec. 1, 2021, in the journal Science Translational Medicine, Johns Hopkins Medicine investigators, in collaboration with researchers at three other institutions, circumvented the drug monitoring problem by using positron emission tomography — commonly known as a PET scan — to “see” rifampin’s movement in a living body.
“We imaged patients with or without orthopaedic implant-associated Staphylococcus aureus infections to show that we could visualize how much rifampin actually penetrates the bone,” says study lead author Oren Gordon, M.D., Ph.D., a pediatric infectious diseases fellow at Johns Hopkins Children’s Center and the Johns Hopkins University School of Medicine. “Then, we used the same procedure on mice bred to mimic Staphylococcus bone infections in humans to define how much rifampin would be needed over time to effectively and safely treat the condition.”
The patient imaging studies demonstrated that the concentration of rifampin penetrating into bone is only about 14% — or about one-third — as much as previously believed.
“Taking the results back to the animal model, we determined that giving the mice about three times the currently used rifampin dose substantially increased bone concentration and achieved higher bacterial killing,” says study senior author Sanjay Jain, M.D., professor of pediatrics, and of radiology and radiological sciences at the Johns Hopkins University School of Medicine; and professor of international health at the Johns Hopkins Bloomberg School of Public Health. “We also learned that treating the infections with four weeks of combination antibiotic therapy — including the higher dose of rifampin — was as efficient as the standard six-week treatment using the traditionally prescribed dose.”
“Moreover, the shorter, higher-dose regimen also resulted in fewer antibiotic-resistant strains of Staphylococcus aureus arising in the mice,” adds Gordon.
“The good news is that the higher doses of rifampin that worked well in the animal model are known to be safe for humans,” says Jain. “However, additional studies are needed to confirm the absolute safety and efficacy of this strategy for the treatment of orthopaedic implant-associated infections, including Staphylococcus aureus and its dangerous variant, methicillin-resistant Staphylococcus aureus [better known by its acronym, MRSA].”
Along with Gordon and Jain, the members of the research team from Johns Hopkins Medicine and the Johns Hopkins Bloomberg School of Public Health are Nathan Archer, Robert Dannals, Kimberly Davis, Dustin Dikeman, Bessie Liu, Martin Lodge, Lloyd Miller, Alvaro Ordonez, Steven Rowe, Camilo Ruiz-Bedoya, Babar Shafiq, Paul Sponseller and John Thompson. The researchers participating from other institutions are Jogarao Gobburu, Brooke Langevin and Donald Lee at the University of Maryland School of Pharmacy, Timothy Read at Emory University and Charles Peloquin at the University of Florida College of Pharmacy.
The study was funded by five National Institutes of Health awards: the Director’s Transformative Research Award R01-EB020539, grant R01-HL131829, grant R01-EB025985, R01-A1153349 and T32A1052071.
The authors do not have financial or conflict of interest disclosures related to this study.
Media Contact
Michael E. Newman
Johns Hopkins Medicine
mnewma25@jhmi.edu
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Innovative 3D printed scaffolds offer new hope for bone healing
Researchers at the Institute for Bioengineering of Catalonia have developed novel 3D printed PLA-CaP scaffolds that promote blood vessel formation, ensuring better healing and regeneration of bone tissue. Bone is…

The surprising role of gut infection in Alzheimer’s disease
ASU- and Banner Alzheimer’s Institute-led study implicates link between a common virus and the disease, which travels from the gut to the brain and may be a target for antiviral…

Molecular gardening: New enzymes discovered for protein modification pruning
How deubiquitinases USP53 and USP54 cleave long polyubiquitin chains and how the former is linked to liver disease in children. Deubiquitinases (DUBs) are enzymes used by cells to trim protein…



