Scientists identify novel molecular biomarkers in cells
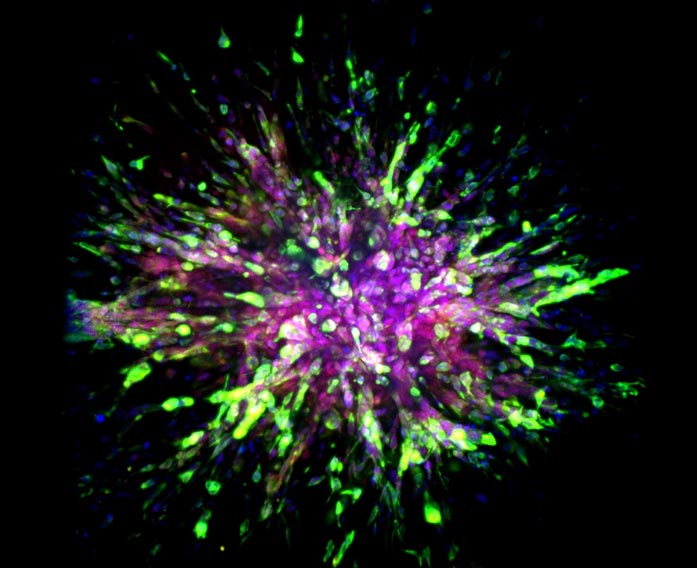
A triple-negative breast cancer organoid invades collagen tissue.
Credit: Eloïse Grasset, Johns Hopkins Medicine
Studying a deadly type of breast cancer called triple negative, Johns Hopkins Medicine scientists say they have identified key molecular differences between cancer cells that cling to an initial tumor and those that venture off to form distant tumors.
The research, using mouse models and human tissues, could pave the way for developing new treatments that target such molecular variations.
A report on the findings is published Aug. 3 in Science Translational Medicine.
“We have long needed new treatment targets and options for triple negative breast cancers,” says Andrew Ewald, Ph.D., the Virginia DeAcetis Professor in Basic Science Research and Director, Department of Cell Biology at the Johns Hopkins University School of Medicine and co-leader of the Cancer Invasion and Metastasis Program at the Johns Hopkins Kimmel Cancer Center. “These cancers often return within three years of diagnosis, and treatments used for other breast cancers don’t typically work for triple negative.”
An estimated 10%–20% of the 280,000 breast cancers diagnosed in the U.S. each year are triple negative, and the rate is higher among African American women, who are twice as likely as others to experience this form of the disease.
The lethal nature of this type of cancer is marked by the fact that its cells lack molecular flags on its surface that connect with the hormones estrogen and progesterone and a cancer growth-promoting protein called Her2-neu. Many current breast cancer therapies work by targeting those flags, rendering them of little use to those with triple negative tumors.
For the current study, the research team looked at molecular differences between initial, or primary, triple-negative breast cancer sites and areas where it spread, or metastatic sites, among three different types of cells: mouse models, human cancers implanted into mice and samples of both primary and metastatic tissues taken from eight patients treated at The Johns Hopkins Hospital.
The researchers used a combination of machine learning, cellular imaging, and biochemical analysis to identify differences in the genetic expression patters of initial and metastatic tumors.
“The bad news from our study is that cells from metastatic sites are super optimized for migration and resisting treatment,” says Ewald. “The good news is that we identified several proteins called transcription factors that these cells require to handle the challenges of migrating and thriving at metastatic sites, and we may be able to design new therapies that target these transcription factors.”
More specifically, Ewald and Johns Hopkins postdoctoral fellow Eloïse Grasset, Ph.D., and others on the research team found several unique properties in the cells of mice engineered to have the mouse-version of triple negative breast cancers, and mice implanted with tumors from people with triple negative breast cancer.
The scientists found that when triple negative breast cancer cells invade other tissues on their way to another part of the body, they gain two cellular properties: better movement and survival.
To do this, breast cancer cells gain a cellular skeleton protein dubbed vimentin, which enhances the migratory ability of so-called mesenchymal cells, a cell type typically found in bones and bone marrow that moves around and makes new cells.
Triple negative breast cancer cells also gain survival advantages by producing a protein called E-cadherin, typically found in epithelial cells that line the ducts and coverings of organs and frequently renew themselves.
When triple negative breast cancer cells gain such survival and migratory qualities, scientists classify their cellular state as so-called hybrid epithelial mesenchymal (EMT) cells.
To look more closely at molecules involved in hybrid EMT states, the scientists sought the help of Elana Fertig, Ph.D., division director and associate director of quantitative sciences and co-director of the Convergence Institute at the Johns Hopkins Kimmel Cancer Center, to track the molecular patterns of individual cells in cell assays that model invasion out of the primary tumor and formation of a colony in a metastatic site.
Fertig’s computational team used machine learning techniques to find patterns among each cell’s expression of RNA, a cousin of DNA involved in protein production. The scientists found that most of the metastatic cells morph into the more mobile, better surviving, hybrid EMT state. Ewald’s team then validated these states in samples from eight patients with triple negative tumors, examining both primary tumors and tissues from metastatic sites of the same patients.
At the molecular level, the most metastatic cells produced five proteins called transcription factors (Grhl2, Foxc2, Zeb1, Zeb2 and Ovol1) that foster the making of proteins involved in either cancer cell invasion or colony formation.
“The molecular differences between metastatic and primary tumors are likely the reason why metastatic tumor cells are so resistant to current treatments,” says Ewald.
His team is studying ways to block the transcription factors’ genes or their resulting proteins to halt metastatic cancer growth as well as whether the same molecular and cellular changes happen in other cancers, such as those in the colon, adrenal glands, stomach, and small intestine.
Other Johns Hopkins researchers who contributed to the study include Matthew Dunworth,Gaurav Sharma, Melanie Loth, Joseph Tandurella, Ashley Cimino-Mathews, Melissa Gentz, Sydney Bracht and Meagan Haynes.
The research was supported by the Breast Cancer Research Foundation, the Twisted Pink Foundation, Hope Scarves, the Jayne Koskinas Ted Giovanis Foundation, the Cindy Rosencrans Fund for Triple Negative Breast Cancer Research and the National Institutes of Health’s National Cancer Institute (U01CA217846, U54CA268083, 3P30CA006973, U01CA212007, U01CA253403).
Journal: Science Translational Medicine
DOI: 10.1126/scitranslmed.abn7571
Media Contacts
Vanessa Wasta
Johns Hopkins Medicine
wasta@jhmi.edu
Office: 410-614-2916
Ayanna Tucker
Johns Hopkins Medicine
atucke25@jhmi.edu
Office: 443-287-8577
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Innovative 3D printed scaffolds offer new hope for bone healing
Researchers at the Institute for Bioengineering of Catalonia have developed novel 3D printed PLA-CaP scaffolds that promote blood vessel formation, ensuring better healing and regeneration of bone tissue. Bone is…

The surprising role of gut infection in Alzheimer’s disease
ASU- and Banner Alzheimer’s Institute-led study implicates link between a common virus and the disease, which travels from the gut to the brain and may be a target for antiviral…

Molecular gardening: New enzymes discovered for protein modification pruning
How deubiquitinases USP53 and USP54 cleave long polyubiquitin chains and how the former is linked to liver disease in children. Deubiquitinases (DUBs) are enzymes used by cells to trim protein…



