Radioguided surgery accurately detects and removes metastatic lymph nodes
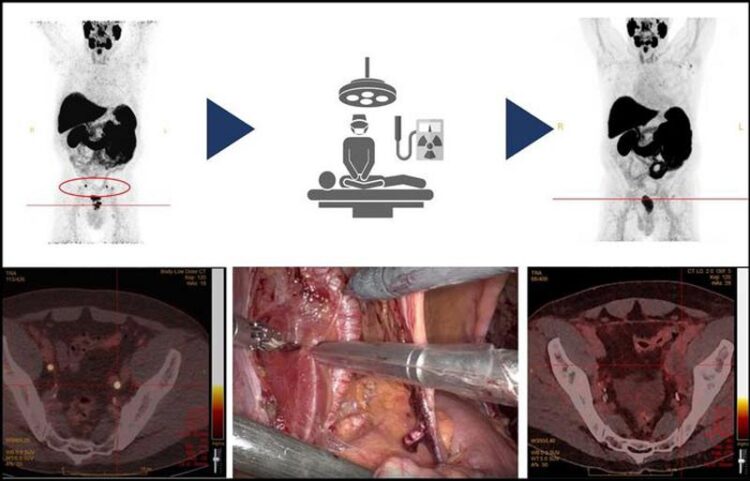
Preoperative (left; top and bottom) and postoperative PSMA-PET/CT images (right; top and bottom) demonstrate the successful removal of two positive pelvic lymph nodes in the radioguided surgical procedure (middle).
Image created by M.G.M. Schilham, Radboud University Medical Centre, Nijmegen, The Netherlands
…in newly diagnosed prostate cancer patients.
Radioguided surgery can detect and remove metastatic pelvic lymph nodes in patients newly diagnosed with prostate cancer, according to research published in the March issue of The Journal of Nuclear Medicine. Targeting the prostate-specific membrane antigen (PSMA), which is overexpressed in most prostate cancer patients, radioguided surgery can improve nodal staging to guide treatment recommendations for this important patient population.
In newly diagnosed prostate cancer patients, nodal involvement correlates with recurrence, and determining if lymph node metastases are present and where they are located is crucial for clinical decision making and treatment planning. For example, patients with nodal involvement can benefit from adjuvant therapies, such as radiation and chemotherapies, which can improve outcomes.
To date, extended pelvic lymph node dissection (ePLND), a procedure in which as many metastatic lymph nodes as possible are removed from the pelvic area, is considered the best tool for nodal staging. Although the therapeutic effect of ePLND in prostate cancer patients is controversial, evidence suggests that removal of all nodal metastases could maximize locoregional disease control.
“PSMA-radioguided surgery can aid the surgeon in accurately finding and removing all metastatic lymph nodes in newly diagnosed prostate cancer patients. This is specifically important to detect positive lymph nodes just outside the standard pelvic surgical area, or in surgically challenging regions, that would have been missed otherwise,” said Diederik M. Somford, MD, PhD, urologist and principal investigator at the Canisius Wilhelmina Hospital in Nijmegen, Netherlands.
The study included 20 newly diagnosed prostate cancer patients with at least one suggestive lymph node visible on a preoperative 18F-PSMA PET/CT scan. 111In-PSMA-radioguided surgery was performed to remove metastatic lymph nodes, and a postoperative 18F-PSMA PET/CT scan was performed to verify successful removal of suggestive lesions. The safety and feasibility of 111In-PSMA-radioguided surgery was assessed, as well as its accuracy in determining metastatic lymph nodes.
No adverse events related to 111In-PSMA-radioguided surgery were reported. 111In-PSMA radioguided surgery identified and removed 29 of 49 lesions, of which 28 (97 percent) contained lymph node metastases. Another 14 of 49 (29 percent) removed lymph nodes were not detected with 111In-PSMA radioguided surgery, of which two contained metastases.
“Although previous studies have reported on the feasibility of PSMA-radioguided pelvic lymph node surgery, this study is among the first trials to investigate this technique in a larger number newly diagnosed patients,” said Melline G.M. Schilham, MD, executive researcher at the Radboud University Medical Centre in Nijmegen, Netherlands. “The study shows that this novel surgical technique is safe and feasible. Furthermore, each patient underwent postoperative imaging to check whether the lymph nodes were truly removed, which is important to substantiate the reliability of the results.”
“The current results demonstrate the great potential for radioguided surgery in prostate cancer and highlight the expanding role of molecular imaging at the operating room,” noted Mark Rijpkema, PhD, principal investigator at the Radboud University Medical Centre. “Optimization of tracers and larger clinical trials may further improve surgical outcomes in the future by implementing both measurements of removed tissue, as well as real-time measurements during surgery.”
The authors of “Prostate-Specific Membrane Antigen–Targeted Radioguided Pelvic Lymph Node Dissection in Newly Diagnosed Prostate Cancer Patients with a Suspicion of Locoregional Lymph Node Metastases: The DETECT Trial” include Melline G.M. Schilham, Department of Medical Imaging, Radboud University Medical Center, Nijmegen, The Netherlands, Prosper Prostate Cancer Clinics, Nijmegen/Eindhoven, The Netherlands, and Department of Urology, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands; Diederik M. Somford and Jean Paul A. van Basten, Prosper Prostate Cancer Clinics, Nijmegen/Eindhoven, The Netherlands, and Department of Urology, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands; Heidi V.N. Küsters-Vandevelde, Department of Pathology, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands; Rick Hermsen, Department of Nuclear Medicine, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands; Robert J. Hoekstra, Prosper Prostate Cancer Clinics, Nijmegen/Eindhoven, The Netherlands, and Department of Urology, Catharina Hospital, Eindhoven, The Netherlands; Tom W.J. Scheenen, Martin Gotthardt, and Mark Rijpkema, Department of Medical Imaging, Radboud University Medical Center, Nijmegen, The Netherlands; and Michiel Sedelaar, Prosper Prostate Cancer Clinics, Nijmegen/Eindhoven, The Netherlands, and Department of Urology, Radboud University Medical Center, Nijmegen, The Netherlands.
Visit the JNM website for the latest research, and follow our new Twitter and Facebook pages @JournalofNucMed or follow us on LinkedIn.
Please visit the SNMMI Media Center for more information about molecular imaging and precision imaging. To schedule an interview with the researchers, please contact Rebecca Maxey at (703) 652-6772 or rmaxey@snmmi.org.
About JNM and the Society of Nuclear Medicine and Molecular Imaging
The Journal of Nuclear Medicine (JNM) is the world’s leading nuclear medicine, molecular imaging and theranostics journal, accessed more than 16 million times each year by practitioners around the globe, providing them with the information they need to advance this rapidly expanding field. Current and past issues of The Journal of Nuclear Medicine can be found online at http://jnm.snmjournals.org.
JNM is published by the Society of Nuclear Medicine and Molecular Imaging (SNMMI), an international scientific and medical organization dedicated to advancing nuclear medicine and molecular imaging—precision medicine that allows diagnosis and treatment to be tailored to individual patients in order to achieve the best possible outcomes. For more information, visit www.snmmi.org.
Journal: Journal of Nuclear Medicine
DOI: 10.2967/jnumed.123.266495
Article Title: Prostate-Specific Membrane Antigen–Targeted Radioguided Pelvic Lymph Node Dissection in Newly Diagnosed Prostate Cancer Patients with a Suspicion of Locoregional Lymph Node Metastases: The DETECT Trial
Article Publication Date: 1-Mar-2024
Media Contact
Rebecca Maxey
Society of Nuclear Medicine and Molecular Imaging
rmaxey@snmmi.org
Office: 703-652-6772
All latest news from the category: Medical Engineering
The development of medical equipment, products and technical procedures is characterized by high research and development costs in a variety of fields related to the study of human medicine.
innovations-report provides informative and stimulating reports and articles on topics ranging from imaging processes, cell and tissue techniques, optical techniques, implants, orthopedic aids, clinical and medical office equipment, dialysis systems and x-ray/radiation monitoring devices to endoscopy, ultrasound, surgical techniques, and dental materials.
Newest articles

Molecular gardening: New enzymes discovered for protein modification pruning
How deubiquitinases USP53 and USP54 cleave long polyubiquitin chains and how the former is linked to liver disease in children. Deubiquitinases (DUBs) are enzymes used by cells to trim protein…

Machine learning accelerates catalyst discovery
Conceptual blueprint to analyze experimental catalyst data. Machine learning (ML) models have recently become popular in the field of heterogeneous catalyst design. The inherent complexity of the interactions between catalyst…

More efficient car designs with AI
8,000 open source models for sustainable mobility. Designing new cars is expensive and time consuming. As a result, manufacturers tend to make only minor changes from one model generation to…



